Services on Demand
Journal
Article
Related links
Share
Ciencias Psicológicas
Print version ISSN 1688-4094On-line version ISSN 1688-4221
Cienc. Psicol. vol.17 no.2 Montevideo Dec. 2023 Epub Dec 01, 2023
https://doi.org/10.22235/cp.v17i2.2630
Original Articles
Sleep quality and daytime sleepiness among college students: testing an explanatory model
1 Universidade Federal de Roraima, Brazil
2 Universidade Federal de Alagoas, Brazil, leogildo.alves.freires@gmail.com
3 Universidade Federal de Roraima, Brazil
4 Universidade Federal de Alagoas, Brazil
The current study aimed to test, through structural equation modeling, an explanatory model of the sleep quality and excessive daytime sleepiness among Brazilian college students (N = 407). They answered the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), 12-item General Health Questionnaire, Fatigue Assessment Scale (FAS), Academic Stress Scale (ASS), Drug Use Time Questionnaire (DUTQ), and demographic information. The bivariate correlations and multiple regressions provided subsidies for the building of an explanatory model that included psychological discomfort, academic stress and the use of caffeine as explanatory variables for predicting sleep quality, and in turn the latter together with fatigue explaining daytime sleepiness. This model showed acceptable fit. The study concludes that higher levels of academic stress, psychological distress, fatigue and caffeine use are associated with lower sleep quality rates among university students. These findings shed light on the importance of considering both individual and contextual variables to understand the sleep-wake cycle in an academic context. These variables should be considered in further studies that aim to apply and evaluate possible future intervention actions.
Keywords: sleep quality; daytime sleepiness; academic stress; undergraduate students.
O presente estudo teve como objetivo testar, através de equações estruturais, um modelo explicativo da qualidade do sono e da sonolência diurna entre estudantes universitários brasileiros (N = 407). Os participantes responderam ao Índice da Qualidade do Sono de Pittsburgh (PSQI), à Escala de Sonolência de Epworth (ESS-BR), ao Questionário de Saúde Geral (QSG-12), à Escala de Avaliação de Fadiga (EAF), à Escala de Estresse Acadêmico (EEA), ao Questionário sobre Tempo de Uso de Drogas (QTUDR) e às informações demográficas. As análises de correlações bivariadas e regressões múltiplas forneceram elementos para a elaboração de um modelo explicativo que incluíram como variáveis explicativas o desconforto psicológico, o estresse acadêmico e o uso de cafeína, como preditores da qualidade do sono e, esta última juntamente com a fadiga, explicando a sonolência diurna. Este modelo apresentou índices adequados de ajuste aos dados empíricos. É possível concluir que maiores níveis de estresse acadêmico, desconforto psicológico, fadiga e uso de cafeína estão associados a menores índices de qualidade do sono entre estudantes universitários. Os resultados demonstram a relevância de considerar variáveis individuais e contextuais para compreender o ciclo vigília-sono no âmbito acadêmico. Essas variáveis devem ser consideradas em futuros estudos que procurem aplicar e avaliar possíveis programas de intervenção.
Palavras-chave: qualidade de sono; sonolência diurna; estresse acadêmico; estudantes universitários.
Este estudio tuvo como objetivo evaluar, vía modelaje por ecuaciones estructurales, un modelo explicativo de la calidad del sueño y somnolencia diurna excesiva en estudiantes universitarios brasileños (N = 407). Los participantes respondieron al Índice de la Calidad del Sueño de Pittsburgh (PSQI), a la Escala de Somnolencia de Epworth (ESS-BR), Cuestionarios de Salud General (QSG-12), la Escala de Evaluación de Fatiga (EAF), la Escala de Estrés Académico (EEA), el Cuestionario sobre el Tiempo de Uso de Drogas (QTUDR) e informaciones demográficas. Los análisis de correlaciones y regresiones ofrecieron respaldo para la elaboración de un modelo explicativo que incluye como variables explicativas el malestar psicológico, el estrés académico y el uso de cafeína como predictores de la calidad de sueño y esta última juntamente con la fatiga, lo que explica la somnolencia diurna. Este modelo presentó índices adecuados de ajuste a los datos empíricos. Se puede concluir que niveles mayores de estrés académico, malestar psicológico, fatiga y uso de cafeína de asocian a índices menores de calidad del sueño entre estudiantes universitarios. Tales resultados ponen en evidencia la importancia de considerar tanto variables individuales cuanto contextuales para entender el ciclo vigilia-sueño en el ámbito académico. Estas variables deben ser consideradas en estudios posteriores que busquen aplicar y evaluar posibles acciones futuras de intervención.
Palabras clave: calidad del sueño; somnolencia diurna; estrés académico; estudiantes universitarios.
The act of sleeping is an active, repetitive and reversible behavior that serves a variety of functions, including restorative, physiological and cognitive processes (Ackermann & Rasch, 2014; Landmann et al., 2014; Rasch & Born, 2015). Consequently, sleep is essential for neurogenesis, synaptic plasticity, attention, wakefulness, learning, and memory consolidation (Panjwani et al., 2019).
Nevertheless, contemporary society is constantly demanding work, study, and social commitments at irregular hours, resulting in a lack of sleep and harm to physical and mental health (Amaro & Dumith, 2018). People prefer to sacrifice some sleep time to deal with the various interests they have on a daily basis, assuming that such a practice will not have adverse or harmful consequences (Curcio et al., 2006).
Students at universities are a good example of this (Almojali et al., 2017). It is generally known that they have an irregular sleep pattern, start and end time of sleep, which occurs later on weekends as compared to weekdays, resulting from social and academic demands, adaptation to university settings, and lack of parental supervision (Amaral, 2018; Araújo et al., 2013; Phillips et al., 2017). As an indication of how severe this phenomenon is, such a pattern results in high variation in sleep habits, resulting in a high sleep debt, which is not frequently observed in non-clinical populations or those who do not work shifts (Lemma et al., 2012; Li et al., 2017).
Several factors affect the learning performance of university students, including sleep quality (SQ) and daytime sleepiness (DS) (Huang et al., 2014). Generally, self-report instruments are used to assess sleep quality based on objective factors (such as nightly awakenings, latency, and sleep duration), as well as subjective factors (such as perception of sleep depth and degree of restoration that individuals feel when they wake up, as well as general satisfaction with sleep; Bertolazi, 2008). The somnolence is usually an increased propensity to nap/fall asleep during the day or an inability to remain alert during the day (Thorpy & Billiard, 2011). In addition, it is usually accompanied by low sleep latency, changes in important sleep stages due to accumulated debt, which are common signs that sleep disorders exist (Kaur & Singh, 2017).
Since sleep, sleep quality, and sleepiness are related to aspects of physical and mental health as well as cognitive aspects of learning and memory, it is thought that the study of conditions that interfere with these variables is a relevant demand for investigation and intervention by the academic community (Christodoulou et al., 2023; Fonseca & Genzel, 2020). In general terms, previous studies have already demonstrated some variables that can predict the quality of sleep and daytime sleepiness in a university population, with emphasis on academic stress (Alotaibi et al., 2020), psychological distress (Najafi Kalyani et al., 2017), fatigue (Sajadi et al., 2014), as well as the use or abuse of psychoactive substances (Zhabenko et al., 2016).
With regard to the phenomenon of stress, this is conceived as a state of activation of the organism in response to the perception of a threat, real or imagined, that has the potential to change the organism's condition of subjective well-being and cause feelings of discomfort and/or temporary or permanent discomfort (Lazarus & Folkman, 1984). Thus, academic stress (AS) is described as an activation reaction to academic stimuli on a physical, emotional, cognitive, and behavioral level (García & Zea, 2011). Students often perceive taking tests, presenting work in class, being overloaded with assignments, and other situations as stressful (García-Ros et al., 2012; Lund et al., 2010). Previous studies have already shown the adverse effects of AS on the SQ of college students in a wide range of situations (Lemma et al., 2012; Lund et al., 2010).
The construct of psychological distress (DP) refers to a group of non-severe, non-psychotic mental disorders that typically involve the presence of anxiety, depression, substance abuse, and low self-efficacy (Massud et al., 2007), which in turn predicts SQ. In a prospective longitudinal study with Japanese adolescents, Kaneita et al. (2009) found that sleep disturbance increased the likelihood of becoming mentally ill and vice versa. Another body of research has shown that changes in mental health status are closely related to differences in sleep status (Cheng et al., 2012; Suzuki et al., 2011).
The fatigue variable is typically understood as a state of tension, fatigue, or lack of energy (Fujii et al., 2015). According to recent research, fatigue may be a symptom brought on by an unhealthy lifestyle (e.g., sedentary behaviors; Wang et al., 2019), which is a common issue among adults, including university students (Koohsari et al., 2021). As a result, this variable equally affects the SQ in many groups (Wylie et al., 2022). It has been demonstrated that there is a strong correlation between normal fatigue and sleep (in a non-clinical population) as well as a relationship between poor sleep quality, short sleep duration, high levels of stress, and a perception of lower levels of subjective health and sleepiness (Åkerstedt et al., 2014). Another study (Tsai & Lee-Chiong, 2013) shows the significant prevalence of fatigue among persons with sleep disorders, such as insomnia, obstructive sleep apnea, narcolepsy, etc.
In addition, substance use/abuse is another important condition since it implies individual physiological and cognitive consequences that, in turn, interact with the sleep-wake cycle (Madras & Kuhar, 2013). Yet, caffeine has been investigated less frequently (Gillin et al., 2005). In a meta-analysis, Gardiner et al. (2023) showed that caffeine usage significantly reduced efficiency, latency, and total sleep duration. Additionally, there is also evidence that students who consume caffeine have poorer sleep quality (Henriques, 2008). Furthermore, Sin et al. (2009), in a systematic review, demonstrated that caffeine abstinence promotes an increase in sleep quality.
Thus, the current study sought to propose an explanatory model in light of the scenario described through Structural Equation Modeling (SEM) of the SQ and DS of a sample of Brazilian university students: the independent variables are PD, AS, fatigue and the use of psychoactive substances; thus, sleep quality and daytime sleepiness are the model's criterion variables. The proposal of a predictive model is a form of obtaining data to be considered in future intervention actions with regard to the health and academic performance of university students; these data, in turn, play a significant role in enhancing student satisfaction with their overall university experience (Lopes et al., 2013).
Materials and Methods
Participants
Participants were 407 undergraduate students from a public higher education institution in the North Region of Brazil, located in the city of Boa Vista in the Brazilian State of Roraima. Participants ranged in age from 18 to 63 years (M ean = 23 years; SD= 6.75). Most of them were female (64.4%), single (82.1%), attending daytime courses (56%), and studying psychology (26.5%). Regarding substance use/abuse: 80.5% of students used caffeine and 51.6% drank alcohol. In addition, the use of other substances was reported: tobacco (7.8%), amphetamines (2.5%), tranquilizers (1.7%), marijuana (7.1%), cocaine (1%), and inhalants (0.2%).
Measures
Participants answered an online questionnaire that included questions about age, gender, sexual orientation, marital status, religion, substance use, etc.
Pittsburg Sleep Scale Index (PSQI; Buysse et al., 1989). The PSQI assesses the quality of sleep in the last month. The PSQI version adapted for the Brazilian context (Bertolazi, 2008) consists of 19 questions, and evaluates seven sleep components: subjective quality of sleep, sleep latency, sleep duration, sleep efficiency, sleep disorders, medication use, and daytime dysfunction. The score can range from 0 (Very good / No problem at all) to 3 (Very bad / A very big problem) for each component, with a maximum total score of 21 points. In the current study, the response scale was reversed so that the higher the PSQI score, the better the participants' sleep quality. In this study, according to Marôco and Garcia-Marques (2006), the Cronbach's alpha of this measure showed moderate reliability (α = .82).
Epworth Sleepiness Scale (ESS; Johns, 1991). The ESS evaluates the respondent's chances of having dozed off or fallen asleep while engaged in eight different activities in daily life (e.g., “Sitting and reading”, “Watching TV”, etc.). The scale items (i.e., eight items) were answered on a four-point scale (ranging from 0 =would never doze to 4 =high chance of dozing), presenting, in this study, a moderate reliability index, α = .83 (Marôco & Garcia-Marques, 2006). In the present research, we used the ESS’s Brazilian adaptation (Bertolazi et al., 2009).
General Health Questionnaire (GHS-12; Goldberg, 1972). The GHS-12 aims to assess the mental health of people through questions that deal with non-psychotic psychiatric symptoms (e.g., “Have you recently lost much sleep over worry?”). The set of items was answered on a four-point Likert scale, with each item ranging from 0 to 3. For negatively worded items, 0 indicated not at all, 1 indicated seldom, 2 usual and 3 more than usual, while positively worded items were reversely scored. All items were added to obtain the total score, where higher scores indicate worse mental health. In the current study, the reliability index of the GHS-12 was moderate, α = .80 (Marôco & Garcia-Marques, 2006).
Fatigue Assessment Scale (FAS; Michielsen et. al, 2004). The FAS consists of 10 items (e.g., “I am bothered by fatigue”; “I get tired very quickly”, etc.). This set of items was answered on a five-point Likert scale (varying from 1 = never to 5 = always), taking into account how the individual has been feeling in the last few days in relation to fatigue. The reliability index of the FAS, in this study, was moderate, α = .87 (Marôco & Garcia-Marques, 2006).
Academic Stress Scale (ASS). The ASS consists of an adapted version of the Work Stress Scale (WSS; Paschoal & Tamayo, 2004) and was validated for the university context by Freires et al. (2018). Its 12 items (e.g., “The way tasks are distributed between disciplines has made me nervous”) were answered on a five-point Likert-type scale (ranging from 1 = strongly disagree to 5 = strongly agree). In the present study, the internal consistency of the ASS was adequate (α = .88).
Drug Use Time Questionnaire (DUTQ). This questionnaire consists of 27 items and was used to assess the frequency of use of numerous substances: tobacco, amphetamines, stimulants, tranquilizers, alcohol, marijuana, cocaine, crack, and inhalants. Thus, the DUTQ enabled the identification of occasional and dependent users of some of the most common drugs (Mariño et al., 1998).
Procedure
All the participants were recruited through social networks (e.g., Instagram) and answered an online questionnaire through Lime Survey. Each instrument had the necessary instructions to proceed with the answers and was self-administered. Additionally, the collaborating researchers made themselves available through email to address any questions about taking part in the study. Finally, the prerogatives provided for in Resolution No. 510/16 of the Brazilian National Health Council regarding the regulation of research with human beings were respected. The Ethics Committee of a public higher education institution in the North Region of Brazil approved this study (Process No. 726.580, Healthy Sciences Centre).
Data Analysis
Statistical analyses were performed using the R language (R Development Core Team, 2015). Using the Rcommander interface of the Rcmdr package (Fox, 2017), descriptive statistics were carried out to characterize the sample as well as correlation and linear regression analyses (i.e., associations between antecedent variables and criterion variables: SQ and DS).
In order to test the explanatory model, the Lavaan package was used (Rosseel, 2012), by applying the Robust Maximum Likelihood (MLR) estimator. For the model fit, we considered the following fit indexes: (a) Chi-square to degrees-of-freedom ratio (S-Bχ2/df), accepting values between 2 and 3, admitting up to 5; (b) Comparative Fit Index (CFI) and Tucker-Lewis index (TLI), which should be greater than .90; (c) Standardized Root Mean Square Residual (SRMR), assuming as recommended a value below .08; and (d) Root Mean Square Error Approximation (RMSEA), with recommended values between .05 and .08, assuming up to .10, where the confidence intervals (90%) do not include a value greater than .10 (Schreiber et al., 2006). With regard to inferential tests, the direct and indirect effects were based on bootstrapped estimates (10.000 bootstrap simulations; Hayes, 2017), which are considered significant when the confidence interval (95%) does not include zero.
Results
Correlates of sleep quality and daytime sleepiness in college students
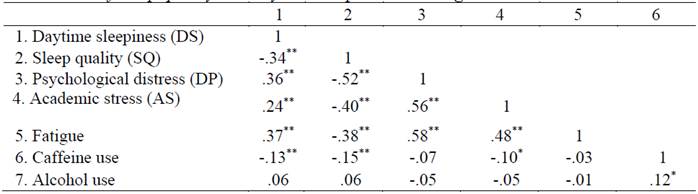
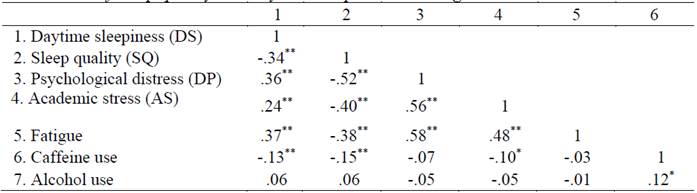
In order to investigate to what extent the independent variables of the present study correlate with the criterion, SQ and DS variables, correlation analyses were performed. With regard to frequency of substance usage, the sample mostly reported the use of caffeine and alcohol; therefore, the other substances were disregarded in the analyses. As can be seen in Table 1, DS was negatively related to SQ. In addition, DS was positively correlated with PD, AS, fatigue; the relationship with caffeine use was negative; there was a non-significant relationship with alcohol use. Finally, SQ was negatively correlated with the following variables: PD, AS, fatigue, and caffeine use; again, alcohol use showed a non-significant relationship.
Predictors of sleep quality and daytime sleepiness in college students
Due to the lack of previous studies that allow consolidating a theoretical elaboration about the SQ in college students, we decided to carry out a multiple linear regression (stepwise method) in order to avoid the multicollinearity effect, aiming to define the significant predictors of the SQ and DS of university students. The antecedent variables were selected, for both criterion variables, based on the significance of their respective correlation coefficients, as well as on the theoretical directionality between them. The results are shown in Table 2.
Table 2: Multiple linear regression of sleep quality and daytime sleepiness in college students
Note: B: Unstandardized coefficients; β: Standardized coefficients; t: t-statistic; p: p-value.
With regard to SQ (Table 2), PD, AS, and caffeine use were significant predictors (negative coefficients). Overall, this set of variables (R = .55, F(3, 404) = 56.94, p < .001) explained 31.2% of outcome variability (adjusted R2). For the second regression model (i.e., DS as criterion variable), fatigue, positively, and SQ, negatively, were significant predictors. Overall, these variables (R = .43, F(2, 406) = 47.25, p <.001) explained 19.1% of outcome variability (adjusted R2).
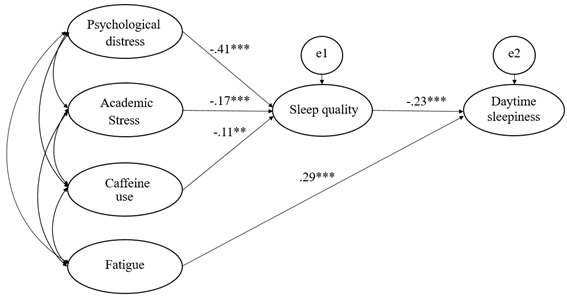
Developing an explanatory model: sleep quality of university students
The results described above suggest that, among university students, SQ and DS can be understood through the levels of AS, PD, fatigue, and caffeine use, taking into account their explanatory power. Based on these results, we proposed a sequence (i.e., an explanatory model) that combines PD, AS, and caffeine use as predictors of SQ. Furthermore, SQ, along with fatigue, jointly explains the DS. Such analytical scenario corresponded to the elaboration of an explanatory model, tested from the SEM, presented in Figure 1.
With regard to the explanatory model statistical adjustment, results indicated adequate fit as follows: χ²/df = 1.14, CFI = .96, TLI = .91, SRMR = .030, and RMSEA = .073 (.031 - .080). Furthermore, the indirect effects were tested. Specifically, PD (β = .09, CI95% = .030 / .082), AS (β = .03, CI95% = .003 / .027), and caffeine use (β = -.03, CI95% = -.498 / -.030) predicted DS through SQ. Finally, the explained variance of the model was determined (Shrout & Bolger, 2002): the model was able to account for 47% of the variance of SQ and DS of university students.
Discussion
Until recently, in empirical studies on sleep patterns and DS among university students, researchers tended to focus solely on measuring the levels of these variables, rather than analyzing potential predictors (Huang et al., 2014; Wang & Bíró, 2021). Thus, the current study aimed to test an explanatory model of SQ and DS in a sample of Brazilian university students through a structural model. The results indicated that PD, AS and caffeine use negatively impacted SQ. Then, SQ (negatively) and fatigue (positively) explained the DS levels of the sample. The fit of the proposed model was considered adequate (Hair et al., 2014), reinforcing the findings of previous studies on the relationship between the aforementioned variables (Alotaibi et al., 2020; Najafi Kalyani et al., 2017; Sajadi et al., 2014; Zhabenko et al., 2016) in a hierarchical manner.
As expected based on previous research, PD was associated with lower levels of SQ in college students. Indeed, cross-sectional epidemiological studies on adult populations demonstrate that mental health conditions play a central role in SQ (Roberts et al., 2000). Sleep dysfunction and/or sleep disorders are the most common symptoms observed in clinical populations, and these symptoms are the motivating factor for seeking professional help (Mendlewicz, 2009). As mentioned, this pattern was also replicated in university students, highlighting that psychological suffering is linked to sleep quality deficits (Wang et al., 2019). Furthermore, there is evidence that sleep problems and mental health status may have a bidirectional relationship: one may be the cause or result of the other (Morphy et al., 2007).
The AS predicted lower levels of SQ among college students, an evidence-replicated finding in the medical-psychological literature (Alotaibi et al., 2020; Yan et al., 2018). Students face sleep problems due to their numerous academic tasks and lack of time for rest (Milojevich & Lukowski, 2016), which is due to pressure for high academic performance (Cardoso et al., 2009). These findings have a biological correlate. Specifically, there are neural connections and proximity between hypothalamic sleep regulatory centres (suprachiasmatic nucleus) and brain structures involved in stress-related autonomic responses (hypothalamic-pituitary-adrenal axis; Tomfohr et al., 2012).
The use of caffeine also had a negative effect on SQ in the structural model tested here. In addition to caffeine's effects on the cardiovascular system, this substance has disruptive effects on sleep, especially when taken in multiple doses throughout the day (Nordt et al., 2012). In addition, caffeine is used as an "insomnia model": the metabolic effects of caffeine, which are physiological in nature, are used to develop a physiological arousal model of chronic insomnia in general samples (Bonnet & Arand, 1992). In terms of physiological correlates, melatonin secretion, the main hormone responsible for sleep synchronization, is controlled by a neurotransmitter affected by caffeine intake (Shilo et al., 2002), which impacts SQ.
Finally, as expected, lower levels of SQ predicted a greater likelihood of DS among college students. Since sleep performs functions in the restoration, protection, and conservation of energy, lower levels of sleep quality translate into losses in the functioning of the individual in the short and long term in their physical, occupational, and cognitive functions (Müller & Guimarães, 2007), which is expressed by daytime sleepiness (i.e., difficulties in maintaining alertness with an adequate level of physiological arousal; Thorpy & Billiard, 2011). It is worth noting that this condition is generally present in more than half of this population, as reported by studies in Brazil with students of dentistry (Angelin et al., 2020), medicine (Milojevich & Lukowski, 2016), and psychology (Danda et al., 2005). In addition, fatigue positively predicted DS. In fact, in non-clinical populations, higher levels of fatigue are associated with higher levels of workload, represented here by academic tasks (Åkerstedt et al., 2014), which, in turn, negatively affect the students' routine, influencing the fulfillment of activities and obligations demanded by the academic context (Zakeri et al., 2006).
Despite the above findings, the present study is not without limitations. Firstly, since the sample was non-probabilistic, generalization of the results to the Brazilian university population is not allowed. Second, the measures used consisted of self-report instruments. Thus, the effect of social desirability on the participants' responses could not be controlled. Finally, another limitation is related to the research design: a cross-sectional study (ex-post facto). In the case of the tested model, although it may be possible to establish a relationship between a set of variables, this does not guarantee the direction (i.e., reverse causality) regarding the influence of a possible third variable (Fife-Schaw, 2010).
In summary, the current findings have implications for the development of future interventions for university populations. At the policy-institutional level, educational institutions can focus on building support networks for the student community (Yusuf et al., 2020), such as customer service, including issues such as resilience training in the face of stressful stimuli (Hasel et al., 2011) and time management in personal and academic activities (Brus, 2006), which can create conditions for an adaptive experience in the academic environment. Thus, future studies could either test the predictive effect of other variables on university students' SQ (e.g., anxiety about falling asleep, sleep hygiene practices, etc.), as indicated by Brown et al. (2002) and Al-Kandari et al. (2017), or investigate the effectiveness of practical interventions with groups of university students from courses with different areas of concentration (Mendes et al., 2019), or from different stages of the academic experience (Soares et al., 2014).
REFERENCES
Ackermann, S. & Rasch, B. (2014). Differential effects of non-REM and REM sleep on memory consolidation? Current Neurology and Neuroscience Reports, 14(2),1-10. https://doi.org/10.1007/s11910-013-0430-8 [ Links ]
Åkerstedt, T., Axelsson, J., Lekander, M., Orsini, N., & Kecklund, G. (2014). Do sleep, stress, and illness explain daily variations in fatigue? A prospective study. Journal of Psychosomatic Research, 76(4), 280-285. https://doi.org/10.1016/j.jpsychores.2014.01.005 [ Links ]
Al-Kandari, S., Alsalem, A., Al-Mutairi, S., Al-Lumai, D., Dawoud, D., & Moussa, M. (2017). Association between sleep hygiene awareness and practice with sleep quality among Kuwait University students. Sleep Health, 3(5), 342-347. https://doi.org/10.1016/j.sleh.2017.06.004 [ Links ]
Almojali, A. I., Almalki, S. A., Alothman, A. S., Masuadi, E. M., & Alaqeel, M. K. (2017). The prevalence and association of stress with sleep quality among medical students. Journal of Epidemiology and Global Health, 7(3), 169-174. http://dx.doi.org/10.1016/j.jegh.2017.04.005 [ Links ]
Alotaibi, A. D., Alosaimi, F. M., Alajlan, A. A., & Bin Abdulrahman, K. A. (2020). The relationship between sleep quality, stress, and academic performance among medical students. Journal of Family & Community Medicine, 27(1), 23-28. https://doi.org/10.4103/jfcm.JFCM_132_19 [ Links ]
Amaral, A. M. L. (2018). Qualidade do sono, higiene do sono e temperamento: Um estudo com estudantes universitários portugueses (Dissertação de mestrado, Universidade de Lisboa). Repositório da Universidade de Lisboa. http://hdl.handle.net/10451/33273 [ Links ]
Amaro, J. R. M. S. & Dumith, S. C. (2018). Sonolência diurna excessiva e qualidade de vida relacionada à saúde dos professores universitários. Jornal Brasileiro de Psiquiatria, 67(2), 94-100. https://doi.org/10.1590/0047-2085000000191 [ Links ]
Angelin, T. J., Mota, K. R., Santos Júnior, V. E., Silva, L., & Heimer, M. V. (2020). Evaluation of sleep quality and daytime sleepiness in dentistry students. Pesquisa Brasileira em Odontopediatria e Clínica Integrada, 20, 1-7. https://doi.org/10.1590/pboci.2020.122 [ Links ]
Araújo, M. F. M. D., Lima, A. C. S., Alencar, A. M. P. G., Araújo, T. M. D., Fragoaso, L. V. C., & Damasceno, M. M. C. (2013). Evaluación de la calidad del sueño de estudiantes universitarios de Fortaleza-CE. Texto & Contexto-Enfermagem, 22(2), 352-360. https://doi.org/10.1590/S0104-07072013000200011 [ Links ]
Bertolazi, A. N. (2008). Tradução, adaptação cultural e validação de dois instrumentos de avaliação do sono: Escala de Sonolência de Epworth e Índice de Qualidade de Sono de Pittsburgh (Dissertação de doutorado). Universidade Federal do Rio Grande do Sul. [ Links ]
Bertolazi, A. N., Fagondes, S. C., Hoff, L. S., Pedro, V. D., Menna Barreto, S. S., & Johns, M. W. (2009). Validação da escala de sonolência de Epworth em português para uso no Brasil. Jornal Brasileiro de Pneumologia, 35(9), 877-883. https://doi.org/10.1590/S1806-37132009000900009 [ Links ]
Bonnet, M. H. & Arand, D. L. (1992). Caffeine use as a model of acute and chronic insomnia. Sleep, 15(6), 526-536. https://doi.org/10.1093/sleep/15.6.526 [ Links ]
Brown, F. C., Buboltz Jr, W. C., & Soper, B. (2002). Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behavioral Medicine, 28(1), 33-38. http://doi.org/10.1080/08964280209596396 [ Links ]
Brus, C. P. (2006). Seeking balance in graduate school: A realistic expectation or a dangerous dilemma? New Directions for Student Services, 2006(115), 31-45. https://doi.org/10.1002/ss.214 [ Links ]
Buysse, D. J., Reynolds III, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193-213. https://doi.org/10.1016/0165-1781(89)90047-4 [ Links ]
Cardoso, H. C., Bueno, F. C. D. C., Mata, J. C. D., Alves, A. P. R., Jochims, I., Vaz Filho, I. H. R., & Hanna, M. M. (2009). Avaliação da qualidade do sono em estudantes de Medicina. Revista Brasileira de Educação Médica, 33(3), 349-355. https://doi.org/10.1590/S0100-55022009000300005 [ Links ]
Cheng, S. H., Shih, C.-C., Lee, I. H., Hou, Y.-W., Chen, K. C., Chen, K.-T., Yang, Y. K., & Yang, Y. C. (2012). A study on the sleep quality of incoming university students. Psychiatry Research, 197(3), 270-274. https://doi.org/10.1016/j.psychres.2011.08.011 [ Links ]
Christodoulou, N., Maruani, J., d’Ortho, M. -P., Lejoyeux, M., & Geoffroy, P.A. (2023). Sleep quality of medical students and relationships with academic performances. L'Encéphale, 49(1), 9-14. https://doi.org/10.1016/j.encep.2021.09.006 [ Links ]
Curcio, G., Ferrara, M., & De Gennaro, L. (2006). Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews, 10(5), 323-337. https://doi.org/10.1016/j.smrv.2005.11.001 [ Links ]
Danda, G. D. N., Ferreira, G. R., Azenha, M., Souza, K. D., & Bastos, O. (2005). Sleep-wake cycle pattern and excessive daytime sleepiness in medical students. Jornal Brasileiro de Psiquiatria, 54(2), 102-106. [ Links ]
Fife-Schaw, C. (2010). Modelos quasi-experimentais. Em G. M. Breakwell., S, Hammond., J. A. Smith & V. G. Haase (Eds.), Métodos de pesquisa em psicologia (pp. 100-115). Artmed. [ Links ]
Fonseca, A. G. & Genzel, L. (2020). Sleep and academic performance: considering amount, quality and timing. Current Opinion in Behavioral Sciences, 33, 65-71. https://doi.org/10.1016/j.cobeha.2019.12.008 [ Links ]
Fox, J. (2017). Using the R Commander: A Point-and-Click Interface or R. Chapman and Hall/CRC Press. [ Links ]
Freires, L. A., Sousa, E. A., Loureto, G. D. L., Monteiro, R. P., & Gouveia, V. V. (2018). Estresse acadêmico: adaptação e evidências psicométricas de uma medida. Psicologia em Pesquisa, 12(3), 22-32. https://dx.doi.org/10.24879/2018001200300532 [ Links ]
Fujii, H., Fukuda, S., Narumi, D., Ihara, T., & Watanabe, Y. (2015). Fatigue and sleep under large summer temperature differences. Environmental Research, 138, 17-21. https://doi.org/10.1016/j.envres.2015.02.006 [ Links ]
García, N. B. & Zea, R. M. (2011). Estrés Académico. Revista de Psicología Universidad Antioquia, 3(2), 65-82. [ Links ]
García-Ros, R., Pérez-González, F., Pérez-Blasco, J., & Natividad, L. A. (2012). Evaluación del estrés académico en estudiantes de nueva incorporación a la universidad. Revista Latinoamericana de Psicología, 44(2), 143-154. [ Links ]
Gardiner, C., Weakley, J., Burke, L. M., Roach, G. D., Sargent, C., Maniar, N., Townshend, A., & Halson, S. L. (2023). The effect of caffeine on subsequent sleep: A systematic review and meta-analysis. Sleep Medicine Reviews, 69, 101764. http://doi.org/10.1016/j.smrv.2023.101764 [ Links ]
Gillin, J. C., Drummond, S. P. A., Clark, C. P., & Moore, P. (2005). Medication and substance abuse. Em M. H. Krygier, T. Roth & W. C. Dement (Eds.), Principles and Practice of Sleep Medicine (4a ed., pp. 1345-1358). Saunders. [ Links ]
Goldberg, D. (1972). The Detection of Psychiatric Illness by Questionnarie. Oxford United Press. [ Links ]
Hair, Jr., Black, W. C., Babin, B. J., & Anderson, R. E. (2014). Multivariate Data Analysis (7a ed.). Pearson Education Limited. [ Links ]
Hasel, K. M., Abdolhoseini, A., & Ganji, P. (2011). Hardiness training and perceived stress among college students. Procedia-Social and Behavioral Sciences, 30, 1354-1358. http://doi.org/10.1016/j.sbspro.2011.10.262 [ Links ]
Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications. [ Links ]
Henriques, A. P. F. C. M. (2008). Caracterização do sono dos estudantes universitários do Instituto Superior Técnico (Dissertação de mestrado). Universidade de Lisboa. [ Links ]
Huang, C. F., Yang, L. Y., Wu, L. M., Liu, Y., & Chen, H. M. (2014). Determinants of daytime sleepiness in first-year nursing students: a questionnaire survey. Nurse education today, 34(6), 1048-1053. http://doi.org/10.1016/j.nedt.2013.11.005 [ Links ]
Johns, M. W. (1991). A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep, 14(6), 540-545. https://doi.org/10.1093/sleep/14.6.540 [ Links ]
Kaneita, Y., Yokoyama, E., Harano, S., Tamaki, T., Suzuki, H., Munezawa, T., Nakajima, H., Asai, T., & Ohida, T. (2009). Associations between sleep disturbance and mental health status: A longitudinal study of Japanese junior high school students. Sleep Medicine, 10(7), 780-786. https://doi.org/10.1016/j.sleep.2008.06.014 [ Links ]
Kaur, F. & Singh, A. (2017). Excessive daytime sleepiness and its pattern among Indian college students. Sleep Medicine, 29, 23-28. https://doi.org/10.1016/j.sleep.2016.08.020 [ Links ]
Koohsari, M. J., Nakaya, T., McCormack, G. R., Shibata, A., Ishii, K., & Oka, K. (2021). Changes in workers' sedentary and physical activity behaviors in response to the COVID-19 pandemic and their relationships with fatigue: longitudinal online study. JMIR Public Health and Surveillance, 7(3), e26293. https://doi.org/10.2196/26293 [ Links ]
Landmann, N., Kuhn, M., Piosczyk, H., Feige, B., Baglioni, C., Spiegelhalder, K., Frase, L., Riemann, D., Sterr. A., & Nissen, C. (2014). The reorganisation of memory during sleep. Sleep Medicine Reviews, 18(6), 531-541. https://doi.org/10.1016/j.smrv.2014.03.005 [ Links ]
Lazarus, R. S. & Folkman, S. (1984). Stress, appraisal, and coping. Springer. [ Links ]
Lemma, S., Gelaye, B., Berhane, Y., Worku, A., & Williams, M. A. (2012). Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sectional study. BMC psychiatry, 12(1), 1-7. https://doi.org/10.1186/1471-244X-12-237 [ Links ]
Li, L., Wang, Y., Wang, S., Li L., Lu, L., Ng, C. H., Ungvari, G. S., Chiu, H. F. K, Hou, C., Jia, F. & Xiang, Y. (2017). Sleep Duration and Sleep Patterns in Chinese University Students: A Comprehensive Meta-Analysis. Journal of Clinical Sleep Medicine, 13(10), 1153-1162. https://doi.org/10.5664/jcsm.6760 [ Links ]
Lopes, E., Milheiro, I., & Maia, A. (2013). Sleep quality in college students: a study about the contribution of lifestyle, academic performance and general well-being. Sleep Medicine, 14(1). https://doi.org/10.1016/j.sleep.2013.11.437 [ Links ]
Lund, H. G., Reider, B. D., Whiting, A. B., & Prichard, J. R. (2010). Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health, 46(2), 124-132. https://doi.org/10.1016/j.jadohealth.2009.06.016 [ Links ]
Madras, B. & Kuhar, M. (Eds.). (2013). The effects of drug abuse on the human nervous system. Elsevier. [ Links ]
Mariño, M. C., González-Forteza, C., Andrade, P., & Medina-Mora, M. E. (1998). Validación de un cuestionario para detectar adolescentes con problemas por el uso de drogas. Salud mental, 21(1), 27-36. [ Links ]
Marôco, J. & Garcia-Marques, T. (2006). Qual a fiabilidade do alfa de Cronbach? Questões antigas e soluções modernas? Laboratório de psicologia, 4(1), 65-90. https://doi.org/10.14417/lp.763 [ Links ]
Massud, M., Barbosa, G. A., & Gouveia, V. V. (2007). Indicadores de saúde mental. Em G. A. Barbosa (Coord.), A saúde dos médicos no Brasil (pp. 143-157). Conselho Federal de Medicina. [ Links ]
Mendes, J., Sousa, M., Leite, V. M., Belchior, N., & Medeiros, T. (2019). Qualidade do sono e sonolência em estudantes do ensino superior. Revista Portuguesa de Investigação Comportamental e Social, 5(2), 38-48. https://doi.org/10.31211/rpics.2019.5.2.150 [ Links ]
Mendlewicz, J. (2009). Sleep disturbances: core symptoms of major depressive disorder rather than associated or comorbid disorders. The World Journal of Biological Psychiatry, 10(4), 269-275. https://doi.org/10.3109/15622970802503086 [ Links ]
Michielsen, H. J., De Vries, J., Van Heck, G. L., Van de Vijver, F. J., & Sijtsma, K. (2004). Examination of the dimensionality of fatigue. The construction of the Fatigue Assessment Scale (FAS). European Journal of Psychological Assessment, 20(1), 39-48. https://doi.org/10.1027/1015-5759.20.1.39 [ Links ]
Milojevich, H. M. & Lukowski, A. F. (2016). Sleep and mental health in undergraduate students with generally healthy sleep habits. PloS one, 11(6), 1-14. http://doi.org/10.1371/journal.pone.0156372 [ Links ]
Morphy, H., Dunn, K. M., Lewis, M., Boardman, H. F., & Croft, P. R. (2007). Epidemiology of insomnia: a longitudinal study in a UK population. Sleep, 30(3), 274-280. https://doi.org/10.1093/sleep/30.3.274 [ Links ]
Müller, M. R. & Guimarães, S. S. (2007). Sleep disorders impact on daily functioning and life quality. Estudos de Psicologia, 24(4), 519-528. https://doi.org/10.1590/S0103-166X2007000400011 [ Links ]
Najafi Kalyani, M., Jamshidi, N., Salami, J., & Pourjam, E. (2017). Investigation of the relationship between psychological variables and sleep quality in students of medical sciences. Depression Research and Treatment, 2017, 1-6. https://doi.org/10.1155/2017/7143547 [ Links ]
Nordt, S. P., Vilke, G. M., Clark, R. F., Cantrell, F. L., Chan, T. C., Galinato, M., Nguyen, V. & Castillo, E. M. (2012). Energy drink use and adverse effects among emergency department patients. Journal of community health, 37(5), 976-981. https://doi.org/10.1007/s10900-012-9549-9 [ Links ]
Panjwani, U., Wadhwa, M., Ray, K., & Kishore, K. (2019). Sleep deprivation, cognitive functions, and countermeasures. Em S. K. Jha & V. M. Jha (Eds.), Sleep, memory and synaptic plasticity (pp. 41-56). Springer. [ Links ]
Paschoal, T. & Tamayo, Á. (2004). Validação da escala de estresse no trabalho. Estudos de Psicologia, 9(1), 45-52. https://doi.org/10.1590/S1413-294X2004000100006 [ Links ]
Phillips, A. J. K., Clerx, W. M., O’Brien, C. S., Sano, A., Barger, L. K., Picard, R. W., Lockley, S. W., Klerman, E. B. & Czeisler, C. A. (2017). Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Scientific Reports, 7(1), 1-13. https://doi.org/10.1038/s41598-017-03171-4 [ Links ]
R Development Core Team. (2015). R: A language and environment for statistical computing (Version 4.3.1). https://cran.r-project.org/doc/manuals/fullrefman.pdf [ Links ]
Rasch, B. & Born, J. (2015). In search of a role of REM sleep in memory formation (Editorial). Neurobiology of Learning and Memory, 122, 1-3. https://doi.org/10.1016/j.nlm.2015.04.012 [ Links ]
Roberts, R. E., Shema, S. J., Kaplan, G. A., & Strawbridge, W. J. (2000). Sleep complaints and depression in an aging cohort: a prospective perspective. American Journal of Psychiatry, 157(1), 81-88. https://doi.org/10.1176/ajp.157.1.81 [ Links ]
Rosseel, Y. (2012). Lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(2), 1-36. http://doi.org/10.18637/jss.v048.i02 [ Links ]
Sajadi, A., Farsi, Z., & Rajai, N. (2014). The relationship between sleep quality with fatigue severity and academic performance of nursing students. Nursing Practice Today, 1(4), 213-220. [ Links ]
Schreiber, J. B., Nora, A., Stage, F. K., Barlow, E. A., & King, J. (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research, 99(6), 323-338. https://doi.org/10.3200/JOER.99.6.323-338 [ Links ]
Shilo, L., Sabbah, H., Hadari, R., Kovatz, S., Weinberg, U., Dolev, S., Dagan, Y. & Shenkman, L. (2002). The effects of coffee consumption on sleep and melatonin secretion. Sleep Medicine, 3(3), 271-273. https://doi.org/10.1016/S1389-9457(02)00015-1 [ Links ]
Shrout, P. E. & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods, 7(4), 422. https://doi.org/10.1037/1082-989X.7.4.422 [ Links ]
Sin, C. W., Ho, J. S., & Chung, J. W. (2009). Systematic review on the effectiveness of caffeine abstinence on the quality of sleep. Journal of Clinical Nursing, 18(1), 13-21. https://doi.org/10.1111/j.1365-2702.2008.02375.x [ Links ]
Soares, A. M., Pereira, M., & Canavarro, J. P. (2014). Saúde e qualidade de vid ana transição para o Ensino Superior. Psicologia, Saúde & Doenças, 15(2), 356-379. http://dx.doi.org/10.15309/14psd150204 [ Links ]
Suzuki, H., Kaneita, Y., Osaki, Y., Minowa, M., Kanda, H., Suzuki, K., Wada, K., Hayashi, K., Tanihata, T & Ohida, T. (2011). Clarification of the factor structure of the 12-item General Health Questionnaire among Japanese adolescents and associated sleep status. Psychiatry research, 188(1), 138-146. https://doi.org/10.1016/j.psychres.2010.10.025 [ Links ]
Thorpy, M. J. & Billiard, M. (Eds.). (2011). Sleepiness: causes, consequences and treatment. Cambridge University Press. [ Links ]
Tomfohr, L. M., Edwards, K. M., & Dimsdale, J. E. (2012). Is obstructive sleep apnea associated with cortisol levels? A systematic review of the research evidence. Sleep Medicine Reviews, 16(3), 243-249. https://doi.org/10.1016/j.smrv.2011.05.003 [ Links ]
Tsai, S. C. & Lee-Chiong, T. (2013). Sleep disorders and fatigue. Sleep Medicine Clinics, 8(2), 235-239. https://doi.org/10.1016/j.jsmc.2013.02.003 [ Links ]
Wang, F. & Bíró, É. (2021). Determinants of sleep quality in college students: a literature review. Explore, 17(2), 170-177. https://doi.org/10.1016/j.explore.2020.11.003 [ Links ]
Wang, K., Xue, Y., Fan, X., Huang, T., & Chen, Z. (2019). Sedentary behaviors, psychological status, and sleep quality in Chinese university students. Social Behavior and Personality, 47(1), 1-10. https://doi.org/10.2224/sbp.7446 [ Links ]
Wylie, G. R., Pra Sisto, A. J., Genova, H. M., & DeLuca, J. (2022). Fatigue across the lifespan in men and women: State vs. trait. Frontiers in Human Neuroscience, 16, 790006. https://doi.org/10.3389/fnhum.2022.790006 [ Links ]
Yan, Y., Lin, R., & Su, Y. (2018). The relationship between adolescent academic stress and sleep quality: a multiple mediation model. Social Behavior and Personality, 46(1), 63-78. https://doi.org/10.2224/sbp.6530 [ Links ]
Yusuf, J. E., Saitgalina, M., & Chapman, D. W. (2020). Work-life balance and well-being of graduate students. Journal of Public Affairs Education, 26(4), 458-483. https://doi.org/10.1080/15236803.2020.1771990 [ Links ]
Zakeri, M., Shaban, M., Kazemnezhad, A., & Tavassoli, K. (2006). Effect of exercise utilizing the rate of respiratory on fatigue in patient with chronic obstructive pulmonary disease. Hayat, 3(30), 17-25. [ Links ]
Zhabenko, O., Austic, E., Conroy, D. A., Ehrlich, P., Singh, V., Epstein-Ngo, Q., Cunningham, R. M. & Walton, M. A. (2016). Substance use as a risk factor for sleep problems among adolescents presenting to the emergency department. Journal of Addiction Medicine, 10(5), 331. http://doi.org/10.1097/ADM.0000000000000243 [ Links ]
How to cite: Sousa, E. A., Freires, L. A., Loureto, G. D. L., & Costa, J. C. A. (2023). Sleep quality and daytime sleepiness among college students: testing an explanatory model. Ciencias Psicológicas, 17(2), e-2630. https://doi.org/10.22235/cp.v17i2.2630
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. E. A. S. has contributed in a, b, c, d, e; L. A. F. in a, b, c, d, e; G. D. L. L. in c, d, e; J. C. A. C. in c, d, e.
Received: July 13, 2021; Accepted: July 24, 2023











 text in
text in