Services on Demand
Journal
Article
Related links
Share
Ciencias Psicológicas
Print version ISSN 1688-4094On-line version ISSN 1688-4221
Cienc. Psicol. vol.17 no.1 Montevideo 2023 Epub June 01, 2023
https://doi.org/10.22235/cp.v17i1.2848
Original Articles
Communication model of condom use in men
1 Universidad Nacional Autónoma de México, México, ricardo.sanchez@iztacala.unam.mx
2 Universidad Nacional Autónoma de México, México
3 Universidad Nacional Autónoma de México, México
4 Universidad Nacional Autónoma de México, México
5 Universidad Nacional Autónoma de México, México
This research proposes a model of communication factors (content, style, context, and time) on consistent condom use in men. A total of one thousand five hundred twenty-four men answered a survey and participated through purposive sampling. Subsequently, three groups were formed: one with participants with an HIV diagnosis, another with those who have taken an HIV test but got a negative result, and the last with those who have never had an HIV detection test. We tested the model’s adjustment in all the samples and then per group through modeling structural equations. We adequately adjusted the first model that considered all the participants. The results were similar when doing this same analysis per group, although, in the case of men with HIV, we included the time they were diagnosed for a better model adjustment. The results are discussed in terms of the empirical evidence of the model and the design of intervention programs that promote condom use in men.
Keywords: communication; condom; HIV infections; men; structural equation models
El propósito de la presente investigación es proponer un modelo de los factores de la comunicación (contenido, estilo, contexto y tiempo) sobre la consistencia en el uso del condón en hombres. Participaron 1524 hombres a través de un muestreo intencionado a quienes se les invitó a responder una encuesta, posteriormente se formaron tres grupos, con diagnóstico de VIH, que se han realizado una prueba de VIH pero que su resultado es negativo, y que nunca se han hecho una prueba de detección. A través del modelamiento de ecuaciones estructurales se probó el ajuste del modelo en toda la muestra y por grupo. El primer modelo que consideró a todos los participantes se ajustó adecuadamente, al hacer este mismo análisis por grupo, los resultados fueron similares, aunque en el caso de los hombres con VIH se incorporó el tiempo de diagnóstico de VIH para un mejor ajuste del modelo. Los resultados se discuten en términos de la evidencia empírica del modelo y del diseño de programas de intervención que promuevan el uso del condón en hombres.
Palabras clave: comunicación; condón; infecciones por VIH; hombres; modelos de ecuaciones estructurales
O propósito da presente investigação é propor um modelo de fatores de comunicação (conteúdo, estilo, contexto e tempo) sobre a consistência no uso do preservativo em homens. Participaram 1524 homens por meio de uma amostragem intencional, os quais foram convidados a responder uma pesquisa, posteriormente foram formados três grupos, com diagnóstico de HIV; que realizaram um teste de HIV, mas que seu resultado foi negativo; e que nunca fizeram um teste de detecção. Por meio da modelagem de equações estruturais, foi testado o ajuste do modelo em toda a amostra e por grupo. O primeiro modelo que considerou todos os participantes foi adequadamente ajustado, ao fazer a mesma análise por grupo, os resultados foram semelhantes, embora no caso dos homens com HIV, o tempo de diagnóstico de HIV tenha sido incorporado para um melhor ajuste do modelo. Os resultados são discutidos em termos da evidência empírica do modelo e do desenho de programas de intervenção que promovam o uso do preservativo em homens.
Palavras-chave: comunicação; preservativo; infecções por HIV; homens; modelos de equações estruturais
Currently, infection from the human immunodeficiency virus (HIV) is considered a chronic disease that causes acquired immunodeficiency syndrome (AIDS). This means that carriers can live longer with an undetectable viral load, improving their life quality as long as they adhere to treatment (Reis et al., 2020). As a result, they are expected to have good emotional and sexual health that helps reduce problems such as stress, anxiety, or depression (Nguyen et al., 2021). Moreover, treatment promotes responsible sexual health to reduce new HIV infections or re-infections (Slurink et al., 2020).
According to the World Health Organization (WHO, 2006, p. 10), sexual health is a “state of physical, mental and social well-being regarding sexuality, and it does not refer only to the absence of disease, dysfunction or discomfort”. The purpose is that people living with HIV can continue enjoying a pleasant sexual life. To achieve this, they should use pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP). Correct and consistent condom use is one of the most widespread and essential strategies, although knowledge and access to condoms could be scarce (Sousa et al. (2021). The proper use of it depends on the ability to place the condom on the penis from beginning to end during the sexual encounter, avoiding its breaking or slipping and the exchange of fluids. Consistency refers to using a condom in every penetrative sexual intercourse (Triana et al., 2017; Villa-Paleo & Carranza-Madrigal, 2017; Zhang et al., 2021b).
Furthermore, condoms have multiple advantages (Beksinska et al., 2020). First, they provide triple protection to prevent HIV and other sexually transmitted infections (STIs) and pregnancy. People can get them without a prescription; they are free and generally available outside health facilities.
Health psychology explains how psychosocial or behavioral variables predict condom use in sexual intercourse (Enríquez et al., 2011). The communication established with the couple is one of the main variables studied, highlighting the impact on interpersonal relationships and health (Manning, 2021). Also, this is a good predictor of condom use in sexual intercourse, mainly when negotiating its use (Chowdhuri et al., 2019; Muhindo et al., 2018; Pysmenna et al., 2020; Zhang et al., 2021a).
Generally, communication assessment focuses on two large areas: on how often men talk to their partner about sexual topics (Craddock et al., 2020; Li & Samp, 2019) and the styles they use to negotiate condom use in sexual intercourse (Decker et al., 2020; Peasant et al., 2015). Although the results are consistent, according to Dixson (1995) and later Muhwezi et al. (2015) and Rogers (2017), communication is a multidimensional process, and its evaluation should so consider it. They state the following five components to be considered:
1.Content refers to the messages or information transmitted and generally focuses on issues related to prevention and sexual health care.
2.Extension, in sexual communication, refers to how often partners communicate about the different topics mentioned in the content.
3.Style refers to how partners communicate; although there are ways of doing so, the assertive style has proven to be the best associated with condom use in sexual intercourse (Gause et al., 2018). This refers to expressing emotions, ideas, and opinions in which one seeks to satisfy wishes and rights but simultaneously respect those of others. Negotiating condom use in sexual intercourse would be an example of this.
4.Time indicates when communication is established. Some studies refer to when parents talk to their children about sexual health (before they have an active sexual life or until they have a problem, such as unplanned pregnancy or STI). It also refers to when the couple negotiates condom use (either planning a sexual encounter or when they are about to initiate a sexual one).
5.Context, although it is generally considered the place where communication occurs, these authors refer to it as the individual perception of that relationship. Mainly, a favorable context of communication arises from this model, which refers to people positively valuing how they communicate with their partners.
Although the authors cited above are interested in communication between parents and children, other studies consider communication between couples. Álvaréz and Villaruel (2015) found that in young people, the type of perception of communication they have predicts whether they talk to their partner or not. This applies to both men and women; however, the type of communication differs between them. Women base communication on sexual health, while men do it on showing their partner their sexual satisfaction.
Similar results stated by Dixson (1995) were found in Quinn-Nilas’ research et al. (2015), whose main objective was validating a self-efficacy scale on sexual communication. They reported a relationship between the different components of communication, which means there is a positive relationship between the frequency of sexual communication, the perception of the communication they establish with their partner, and the negotiation of condom use.
These studies show the importance of evaluating each component of sexual communication with a partner, apart from considering the gender differences of the participants, since behavior differs (Qiao et al., 2020). They should also consider that knowledge of the serological status and the diagnosis obtained impact sexual behavior and communication with the partner (Gause et al., 2018; Haas et al., 2020; Rosenberg et al., 2017; Sanchez et al., 2018).
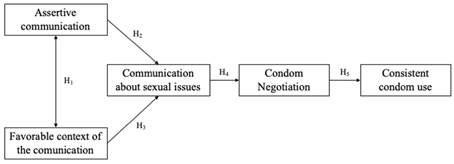
Based on the above, men are infected to a greater extent, according to the statistics reported by the Joint United Nations Program on HIV/AIDS (UNAIDS, 2021). Thus, this research aims to propose an explanatory model of communication factors (Dixson, 1995) that affects consistent condom use in men. We tested this model in three groups of men associated with knowledge of their HIV status: a) HIV positive (HIV+), b) HIV negative (HIV-), which means they have been tested, but the virus has not been detected in the blood; the last group, c) undiagnosed men, who have never had an HIV detection test. We state the following hypotheses (Figure 1):
H1. Assertive communication and the perception of the favorable context of communication have a reciprocal and positive relationship.
H2. Assertive communication directly and positively affects communication about sexual issues.
H3. The perception of the favorable context of communication directly and positively affects communication on sexual topics.
H4. Communication about sexual issues directly and positively affects condom use negotiation.
H5. Negotiating condom use directly and positively affects consistent condom use in sexual intercourse.
Participants
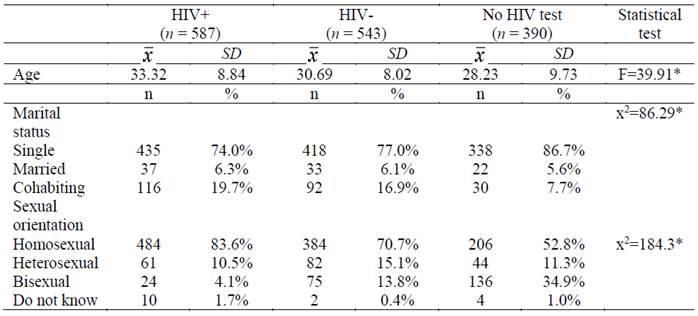
One thousand five hundred and twenty-four men participated in the study through purposive sampling (Pérez-Luco et al., 2017). We contacted users of a care clinic for people with HIV in Mexico and invited people on social media to answer an online survey. The inclusion criteria considered men with an active sexual life and who had sexual intercourse with other men (MSM), while those who rejected informed consent for disseminating their responses at the group level were excluded. Three groups were formed to meet the research objective: 38.8% HIV+ (4.84 years, SD = 5.3 3), 35.6% HIV-, and 25.6% who had never had an HIV detection test. Table 1 shows the participants' sociodemographic characteristics according to their group. There are significant differences between the groups; HIV+ are older than those who have never had an HIV test. Although most are single, men without a detection test represent the highest proportion. Likewise, although most have a homosexual sexual orientation, the HIV+ group shows the highest proportion.
Instruments
Communication scale on sexual issues with the partner: 14 items in Likert-type format with five response options ranging from never to always assess the frequency with which you discuss diverse sexual topics with your partner (example: condom use). The scale has an internal consistency of .90 (Sánchez-Medina et al., 2021).
Scale on sexual communication with the partner: 10 items in Likert-type format with five response options ranging from never to always divided into two factors: assertive communication (example: “I can talk about sexuality”) and the perception of the favorable context of communication (example: “I trust him to talk about my sexual orientation”). The first factor has an internal consistency of .91, and the second of .84. (Sánchez-Medina et al., 2021).
Condom use negotiation strategies scale. The scale of Sánchez-Medina et al. (in press) that evaluates assertive strategies for negotiating condom use with a partner (example: I tell my partner the importance of using a condom for our health), with five items in Likert-type format with five response options ranging from never to always, with an internal consistency of .78.
Consistent condom use. Based on DiClemente and Wingood (1995), we proposed two items that assessed the number of times they had sexual intercourse and how much they used a condom in three months. We obtained a consistency index from these results with values between zero and one. To perform this, we divided the participants’ answers; values equal to one indicate they are consistent in using the condom, while values of zero or close to zero mean they do not use it consistently.
Procedure
The institution of the authors’ origin approved the research protocol, and a specialized clinic to care for HIV patients established an agreement too. Derived from the COVID-19 health contingency, we collected data through an online form shared on social networks. The first part of the survey contained information on informed consent, alluding to confidentiality and anonymity of the information and voluntary participation. The second part corresponded to the request for data demographics and a third of the variables of interest. The estimated response time was half an hour.
Analysis of data
The SPSS statistical package, version 26, was used to conduct descriptive and correlation analyses (Pearson's r). The AMOS program, version 24, was used for structural equations. The indicators to test each proposed model are CFI and GFI with values greater than .95, RMSEA with values less than .050, and TLI with values greater than .90; meeting these criteria shows an adequate model adjustment (Schumacker & Lomax, 2016).
Results
Table 2 presents the means and standard deviations of the variables of communication and negotiation of condom use with the partner and the consistency of this. The results of the total sample and by group are displayed. From the comparison by group, the analysis of differences is presented through the ANOVA test, showing statistically significant differences in assertive communication, the perception of the favorable context of communication, and consistent condom use.
Post hoc analysis found differences in assertive communication between men who have never had an HIV detection test and between those with an HIV+ diagnosis (IJ = .86, p < .05) and with participants from the HIV- group (IJ = -.54, p < .05). In terms of the favorable context of communication, those who had never had an HIV test and the group with HIV+ (IJ = .67, p< .05), and the group HIV- (IJ = .54, p < .05) showed differences between them. In both variables, the mean obtained in those who have never had an HIV test is higher. Regarding consistent condom use, the difference exists between men living with HIV and the other two groups (IJ = .12, p< .001; IJ = .12, p< .001), being those with HIV+, the ones who use a condom more constantly during sexual intercourse.
Table 2: Differences between groups of the variables of the communication model and consistent condom use
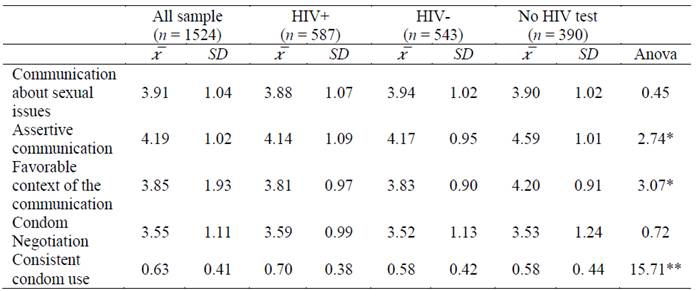
Note:*p < .05 **p < .001
Table 3 presents these results based on Pearson's r regarding the analysis of the relationship between the factors of communication with the partner and consistent condom use. We included the data of the total sample and per comparison group again, showing that when we considered the whole sample and in the case of men living with HIV, the correlations were significant between all the variables. Still, when done by group, this relationship did not appear in some of them; such is the case between the consistent condom use and assertive communication in men in the HIV group and in men who have never had an HIV test.
Table 3: Relationship between communication factors and consistent condom use in men
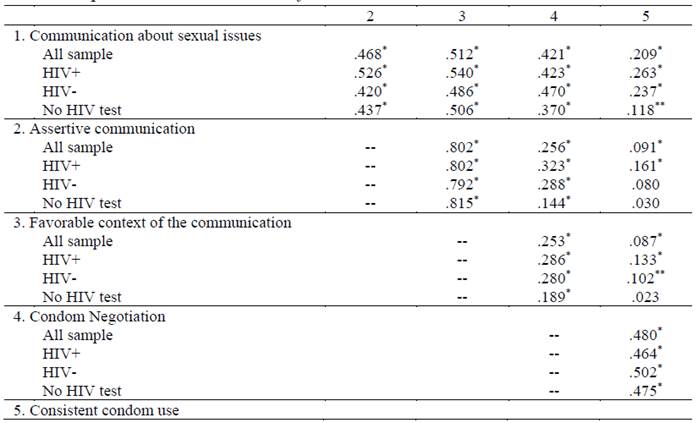
Note: *p < .001. **p < .05
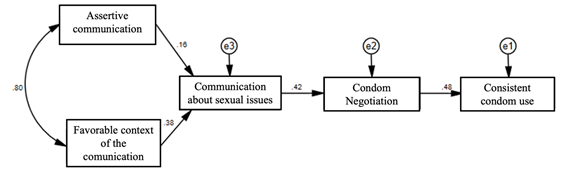
Based on the above, we proposed a communication and negotiation model to explain consistent condom use, initially considering the total sample and later per comparison group. Figure 2 shows the first proposed model, which showed a good fit (x 2 = 12.49; df = 5; p< .05; CFI = .99; RMSEA = .31; GFI = .99; TLI = .99).
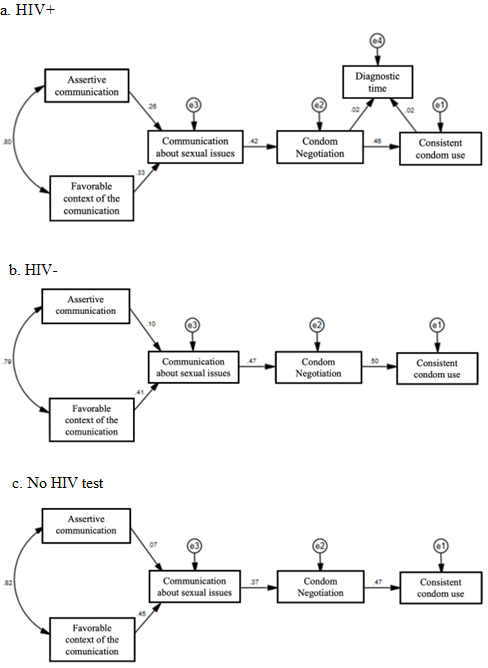
Subsequently, we made a model for each group based on the general one and the results obtained in the analysis of differences and correlation; in all three cases, we found differences to consider (Figure 3). Figure 3 corresponds to men living with HIV; the first model did not show a good fit in terms of the RMSEA values (x 2 = 15.95, df = 5, p< .05; CFI = .99; RMSEA = .06; GFI = .98; TLI = .98). Following the above, we considered diagnosis time as an indirect relationship between the negotiation of consistent condom use as an alternative hypothesis. The model fitted better with incorporating this variable (x 2 = 19.79, df = 5, p < .01; CFI = .98; RMSEA = .05; GFI = .98; TLI = .98).
Figure 3 represents the model of men who have been tested for HIV but are not infected. The results were similar to the model that includes the total sample (x 2 = 11.20, df= 5; p< .05; CFI = .99; RMSEA = .04; GFI = .99; TLI = .98). However, x 2 was not significant (later discussed; x 2 = 3.80, df= 5, p< .57; CFI = 1.00; RMSEA = .00; GFI = .996; TLI = 1.00) in men who have never had an HIV detection test (Figure 3), although the values of the model fit perfectly.
Discussion
This research proposes a model on the communication factors presented by Dixson (1995) and how these influence consistent condom use in men. To do so, we tested a model on the total sample and then per group under three different conditions: men diagnosed with HIV, those who have had an HIV detection test but with a negative result, and men who have never got a test.
Regarding the means obtained in each group, we found significant differences in assertive communication, the perception of the favorable context of communication, and consistent condom use. The foregoing shows that knowledge of the serological status influences some components of communication and sexual behavior. This is congruent with several studies where HIV diagnosis is associated with more preventive sexual behavior than HIV-negative people (Adedimeji et al., 2015). However, as Chen et al. point out, it is necessary to consider that the use of PrEP may be a factor associated with a decrease in condom use, so it is necessary to consider this question in future research and to present whether this effectively influences the differences between groups or not.
We found that the negotiation of condom use (Chowdhuri et al., 2019; Muhindo et al., 2018) had the highest relationship with consistent condom use in the analysis of the correlations between the variables. We also saw this relation between the communication on sexual issues, assertive communication, and the negotiation of condom use. Between the style and the context, the relationships were the highest of all the variables, which is consistent with the proposal made by Dixson (1995).
Based on the stated, we tested a model that considered the different communication components. For this purpose, we proposed five hypotheses that were tested considering the analysis of the relationship between the variables. The first model we proposed considered the total sample, and we found that the evaluation was accurate since it did not require a re-specification of the model (Schumacker & Lomax, 2016). Therefore, based on these findings, we proposed to test it in similar samples or in other groups of men to contribute empirical evidence of the model.
Although the model is verified, we found differences in their characteristics within the demographic data. Thus, considering the analysis of differences and correlation of the groups, we followed the same procedure to know if in each group the model behaved in the same way, this being only for the group of men with an HIV- diagnosis (this means they have been tested for HIV, but the virus has not infected them). Moreover, it is worthwhile to analyze the possible differences in test performance in future research since this could impact their behavior (Haas et al., 2020; Rosenberg et al., 2017).
In contrast, the model initially did not fit adequately in men living with HIV+, and considering the characteristics of the disease, Nguyen et al. (2021) these influence what they do and think. Based on the sociodemographic results, we believed that the diagnosis time could mediate the negotiation of consistent condom use. In concordance with UNAIDS (2021), the foregoing states that sometimes people take time to know their serological status and do not always have access to health services on time. Instead, when detected on time, there is a greater probability of medical attention that can impact sexual behavior (Reis et al., 2020; Sánchez et al., 2018). Considering this, the model adjusted adequately after adding this component.
Moreover, we found that the chi-square test was insignificant in men who had never had an HIV test; therefore, it is necessary to consider other goodness of fit indices, Doral et al. (2018) and Medrano and Muñoz-Navarro (2017). Thus, as a whole, the evidence of the model can receive more significant support.
Based on the model’s results, we consider it necessary to generate more empirical evidence to find if this model can be used in them or what other elements not considered in the present study are suitable to incorporate since having a sexual life active and not taking an HIV test could make them not feel at risk (Chowdhuri et al., 2019).
Finally, we must consider that other elements could mediate these results, Villa-Rueda et al. (2021). Knowledge of HIV, risk perception, skills to reveal serological status, perception of stigma, and access to health services can also influence people with HIV affecting their health. Thus, we recommend broadening the focus of the analysis to identify and recognize how they could mediate or moderate sexual communication and condom use in sexual intercourse.
Conclusions
The evidence of the present research shows a communication model that considers the multidimensional process proposed by Dixson (1995) related to how consistent condom use influences men. The results show empirical evidence of this model; still, it is necessary to continue testing the model in similar samples of men or those with some other particular characteristics and to design interventions to promote condom use in men. We suggest trying the model on women to contribute to this sector of the population not included in the present investigation in the midterm. Moreover, we recommend considering other factors that could be mediating communication and condom use, such as information, skills, and even contextual and cultural variables. To conclude, this model is an approximation that broadens communication analysis from its multidimensionality. Plus, if tested in men with different characteristics, there could be a solution to all the levels of care (primary, secondary, or tertiary) to avoid new HIV infections or re-infections.
REFERENCES
Adedimeji, A. A., Hoover, D. R., Shi, Q., Gard, T., Mutimura, E., Sinayobye, J. d. A., Cohen, M. H., & Anastos, K. (2015). Sexual Behavior and Risk Practices of HIV Positive and HIV Negative Rwandan Women. AIDS and Behavior, 19(7), 1366-1378. https://doi.org/10.1007/s10461-014-0964-z [ Links ]
Álvarez, C. & Villaruel, A. (2015). Association of gender norms, relationship and intrapersonal variables, and acculturation with sexual communication among young adult latinos. Research in Nursing & Health, 38(2), 121-132. https://doi.org/10.1002/nur.21645 [ Links ]
Beksinska, M., Wong, R., & Smit, J. (2020). Male and female condoms: their key role in pregnancy and STI/HIV prevention. Best Practice & Research Clinical Obstetrics & Gynaecology, 66, 55-67. https://doi.org/10.1016/j.bpobgyn.2019.12.001 [ Links ]
Chen, Y.-H., Guigayoma, J., McFarland, W., Snowden, J. M., & Raymond, H. F. (2019). Increases in pre-exposure prophylaxis use and decreases in condom use: behavioral patterns among HIV-negative San Francisco men who have sex with men, 2004-2017. AIDS and Behavior, 23(7), 1841-1845. https://doi.org/10.1007/s10461-018-2299-7 [ Links ]
Chowdhuri, R. N., Pinchoff, J., Boyer, C. B., & Ngo, T. D. (2019). Exploring gender and partner communication: Theory of planned behavior predictors for condom use among urban youth in Zambia. International Journal of Gynecology & Obstetrics, 147(2), 258-267. https://doi.org/10.1002/ijgo.12952 [ Links ]
Craddock, J. B., Barman-Adhikari, A., Combs, K. M., Fulginiti, A., & Rice, E. (2020). Individual and social network correlates of sexual health communication among youth experiencing homelessness. AIDS and Behavior, 24(1), 222-232. https://doi.org/10.1007/s10461-019-02646-x [ Links ]
Decker, M. R., Park, J. N., Allen, S. T., Silberzahn, B., Footer, K., Huettner, S., Galai, N., & Sherman, S. G. (2020). Inconsistent condom use among female sex workers: Partner-specific influences of substance use, violence, and condom coercion. AIDS and Behavior, 24(3), 762-774. https://doi.org/10.1007/s10461-019-02569-7 [ Links ]
Diclemente, R. & Wingood, G. (1995). A randomized controlled trial of an HIV sexual risk reduction intervention for young African American women. Journal of the American Medical Association, 274(16), 1271-1276. https://doi.org/10.1001/jama.1995.03530160023028 [ Links ]
Dixson, M. D. (1995). Models and perspectives of parent-child communication. En T. J. Socha & G. H. Stamp (Eds.), Parents, children, & communication: Frontiers of theory and research (pp. 43-61). Lawrence Erlbaum Associates. [ Links ]
Doral, F., Rodríguez, I., & Meseguer, A. (2018). Modelos de ecuaciones estructurales en investigaciones de ciencias sociales: Experiencia de uso en Facebook. Revista de Ciencias Sociales, 24(1), 22-40. https://doi.org/10.31876/rcs.v24i1.24925 [ Links ]
Enríquez, D., Sánchez, R., & Robles, S. (2011). Teorías y modelos psicológicos sobre el estudio de la salud sexual. En R. Díaz-Loving & S. Robles (Eds.), Salud y sexualidad (pp. 49-84). UNAM-AMEPSO-CONACyT. [ Links ]
Gause, N. K., Brown, J. L., Welge, J., & Northern, N. (2018). Meta-analyses of HIV prevention interventions targeting improved partner communication: effects on partner communication and condom use frequency outcomes. Journal of Behavioral Medicine, 41(4), 423-440. https://doi.org/10.1007/s10865-018-9916-9 [ Links ]
Haas, S. M., Perazzo, J. D., Ruffner, A. H., & Lyons, M. S. (2020). Exploring current stereotypes and norms impacting sexual partner HIV-status communication. Health Communication, 35(11), 1376-1385. https://doi.org/10.1080/10410236.2019.1636340 [ Links ]
Li, Y. & Samp, J. A. (2019). Sexual relationship power, safer sexual communication, and condom use: A comparison of heterosexual young men and women. Western Journal of Communication, 83(1), 58-74. https://doi.org/10.1080/10570314.2017.1398835 [ Links ]
Manning, J. (2021). Communication studies about sex: implications for relationships, health, culture, and identity. A review. Revista Internacional de Información y Comunicación, 30(1), e300114. https://doi.org/10.3145/epi.2021.ene.14 [ Links ]
Medrano, L. A. & Muñoz-Navarro, R. (2017). Aproximación conceptual y práctica a los modelos de ecuaciones estructurales. Revista Digital de Investigación en Docencia Universitaria, 11(1), 219-239. https://doi.org/10.19083/ridu.11.486 [ Links ]
Muhindo, R., Sanyu, B., & Nankumbi, J. (2018). Factors associated with condom use among university female students in Uganda. Journal of Public Health and Disease Preventive, 1(1), 1-8. [ Links ]
Muhwezi, W., Katahoire, A., Banura, C., Mugooha, H., Kwesiga, D., Bastien, S., & Kleep, K. (2015). Perceptions and experiences of adolescents, parents and school administrators regarding adolescents-parents communication on sexual and reproductive health issues in urban and rural Uganda. Reproductive Health, 12, 110. https://doi.org/10.1186/s12978-015-0099-3 [ Links ]
Nguyen, A. L., Sundermann, E., Rubtsova, A. A., Sabbag, S., Umlauf, A., Heaton, R., Letendre, S., Jeste, D. V., & Marquine, M. J. (2021). Emotional health outcomes are influenced by sexual minority identity and HIV serostatus. AIDS Care, 33(9), 1127-1132. https://doi.org/10.1080/09540121.2020.1785998 [ Links ]
ONUSIDA. (2021). Hoja informativa - Últimas estadísticas sobre el estado de la epidemia de sida. https://www.unaids.org/es/resources/fact-sheet [ Links ]
Organización Mundial de la Salud. (2006). Defining sexual health-Report of a technical consultation on sexual health 28-31 January 2002, Geneva. [ Links ]
Peasant, C., Parra, G. R., & Okwumabua, T. M. (2015). Condom negotiation: findings and future directions. The Journal of Sex Research, 52(4), 470-483. https://doi.org/10.1080/00224499.2013.868861 [ Links ]
Pérez-Luco, R., Lagos, L., Mardones, R., & Sáez, F. (2017). Taxonomía de diseños y muestreo en investigación cualitativa. Un intento de síntesis entre las aproximaciones teórica y emergente Ámbitos Revista Internacional de Comunicación, 39, 1-18. [ Links ]
Pysmenna, O., Korotchenko, S., & Su-I, H. (2020). To use or not to use?: a mixed methods study on predictors and barriers of condom use among college students. International Journal of Multiple Research Approaches, 12(2), 216-233. https://doi.org/10.29034/ijmra.v12n2a4 [ Links ]
Qiao, J., Guo, Y., Zhu, Y., Hong, Y. A., Xu, Z., Zeng, C., Zhang, H., Cai, W., Li, L., Liu, C., & Kellstedt, D. K. (2020). Gender differences in the relationship of sexual partnership characteristics and inconsistent condom use among people living with HIV in China. AIDS Care, 32(1), 128-135. https://doi.org/10.1080/09540121.2019.1622632 [ Links ]
Quinn-Nilas, C., Milhausen, R., Breuer, R., Bailey, J., Pavlou, M., DiClemente, R., & Wingood, G. (2015). Validation of the sexual communication self-efficacy scale. Health Education & Behavior, 43(2), 165-171. https://doi.org/10.1177/1090198115598986 [ Links ]
Reis, A., Lencastre, L., Jonsson, C., & Guerra, M. P. (2020). Treatment adherence, meaning in life and affects in quality of fife of HIV/AIDS patients. Journal of Happiness Studies, 21(7), 2405-2417. https://doi.org/10.1007/s10902-019-00182-y [ Links ]
Rogers, A. (2017). Parent-adolescent sexual communication and adolescents’ sexual behaviors: A conceptual model and systematic review. Adolescent Research Review, 2, 293-313. https://doi.org/10.1007/s40894-016-0049-5 [ Links ]
Rosenberg, M. S., Gómez-Olivé, F. X., Rohr, J. K., Houle, B. C., Kabudula, C. W., Wagner, R. G., Salomon, J. A., Kahn, K., Berkman, L. F., Tollman, S. M., & Bärnighausen, T. (2017). Sexual behaviors and HIV status: A population-based study among older adults in rural South Africa. Journal of acquired immune deficiency syndromes, 74(1), e9-e17. https://doi.org/10.1097/QAI.0000000000001173 [ Links ]
Sánchez, T. H., Zlotorzynska, M., Sineath, R. C., Kahle, E., Tregear, S., & Sullivan, P. S. (2018). National trends in sexual behavior, substance use and HIV testing among United States men who have sex with men recruited online, 2013 through 2017. Aids and Behavior, 22(8), 2413-2425. https://doi.org/10.1007/s10461-018-2168-4 [ Links ]
Sánchez-Medina, R., Bárcena-Gaona, S., Enríquez-Negrete, D. J., & Rosales-Piña, C. R. (en prensa). Validación de la escala de estrategias de negociación sobre el uso del condón en hombres. [ Links ]
Sánchez-Medina, R., Enríquez-Negrete, D.J., Rosales-Piña, C.R., & Pérez-Martínez, P.U. (2021). Diseño y validación de dos escalas de comunicación sexual con la pareja en hombres que tienen sexo con hombres. Pensando Psicología, 17(2), 1-31. https://doi.org/10.16925/2382-3984.2021.02.01 [ Links ]
Schumacker, R. & Lomax, R. (2016). Beginner’s guide to structural equation modeling. Routledge. [ Links ]
Slurink, I., van Benthem, B., van Rooijen, M. S., Achterbergh, R., & van Aar, F. (2020). Latent classes of sexual risk and corresponding STI and HIV positivity among MSM attending centres for sexual health in the Netherlands. Sexually Transmitted Infections, 96(1), 33-39. https://doi.org/10.1136/sextrans-2019-053977 [ Links ]
Sousa, L. R. M., Elias, H. C., Fernandes, N. M., Gir, E., & Reis, R. K. (2021). Knowledge of PEP and PrEP among people living with HIV/aids in Brazil. BMC Public Health, 21(1), 64. https://doi.org/10.1186/s12889-020-10135-3 [ Links ]
Triana, A. Z., Flores, F. R., & Sánchez, A. M. (2017). Negociación en el uso del condon en estudiantes universitarios. Waxapa, 9(17), 19-23. [ Links ]
Villa-Paleo, M. T. & Carranza-Madrigal, J. (2017). Conocimiento del uso correcto del condón masculino en alumnos de preparatoria de una población indígena del estado de Michoacán. Medicina Interna de México, 33(5), 580-604. https://doi.org/10.24245/mim.v33i5.1163 [ Links ]
Villa-Rueda, A., Onofre-Rodríguez, D., Churchill, S., Ramírez-Barajas, F. & Benavides-Torres, R. (2021). Multilevel elements associated with HIV serosorting for sexual encounters: A scoping literature review. Ciência & Saúde Coletiva, 26(6), 2183-2194. https://doi.org/10.1590/1413-81232021266.13142019. [ Links ]
Zhang, W., Choi, E. P. H., Fong, D. Y. T., & Wong, J. Y. H. (2021a). A moderated mediation analysis of condom negotiation and sexual orientation on the relationship between sexual coercion and condom use in Chinese young women: Cross-sectional study. JMIR Public Health Surveill, 7(1), e24269. https://doi.org/10.2196/24269 [ Links ]
Zhang, H., Yu, Q., Li, Z., Xiu, X., Lv, F., Han, M., & Wang, L. (2021b). Efficacy of psychological interventions towards the reduction of high-risk sexual behaviors among people living with HIV: A systematic review and meta-analysis, 2010-2020. AIDS and Behavior, 25(10), 3355-3376. https://doi.org/10.1007/s10461-021-03181-4 [ Links ]
How to cite: Sánchez-Medina, R., Rosales-Piña, C. R., Enríquez-Negrete, D. J., Zuñiga-Rodríguez, M. & Gómez-Lamont, M. F. (2023). Communication model of condom use in men. Ciencias Psicológicas, 17(1), e-2848. https://doi.org/10.22235/cp.v17i1.2848
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. R. S.-M. has contributed in a, b, c, d, e; C. R. R.-P.. in b, c, d, e; D. J. E.-N. in c, d, e; M. Z.-R. in b, d, e; M. F. G.-L. in b, e.
Received: March 07, 2022; Accepted: December 14, 2022











 text in
text in