Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Ciencias Psicológicas
versión impresa ISSN 1688-4094versión On-line ISSN 1688-4221
Cienc. Psicol. vol.16 no.2 Montevideo dic. 2022 Epub 01-Dic-2022
https://doi.org/10.22235/cp.v16i2.2324
Original Articles
Religiosity/spirituality (R/S) in professional practice in pediatric oncology: resource or protocol?
1 Universidade de São Paulo, Brasil, rossatousp@usp.br
2 Universidade de São Paulo, Brasil
3 Universidade de São Paulo, Brasil
4 Universidade de São Paulo, Brasil
The inclusion of religiosity/spirituality (R/S) as a dimension of health care still raises reflections, especially when we analyze professional practices. Thus, this integrative literature review aimed to analyze how pediatric oncology professionals experience R/S in their practices. Through the bases/libraries CINAHL, PsycINFO, Pubmed, SciELO and Lilacs, 12 studies produced between the years of 2009 and 2019 were retrieved, nine qualitative and three quantitative. The results were presented in two thematic categories: 1) R/S as an element that permeates situations experienced at work; 2) R/S as a dimension present in the lives of patients and family members. It became evident that, although pediatric oncology professionals consider R/S as an important dimension in care, it is still understood as a resource used mainly by patients and family members, with predominance, among professionals, as something that is more linked to a protocol than an effective resource for working in the area.
Keywords: health personnel; neoplasms; child; adolescent; spirituality
A inclusão da religiosidade/espiritualidade (R/E) como uma dimensão do cuidado em saúde ainda desperta reflexões, sobretudo quando analisamos as práticas profissionais. Assim, esta revisão integrativa de literatura teve por objetivo analisar como os profissionais da oncologia pediátrica vivenciam a R/E em suas práticas. Pelas bases/bibliotecas CINAHL, PsycINFO, Pubmed, SciELO e Lilacs foram recuperados 12 estudos produzidos entre 2009-2019, sendo nove qualitativos e três quantitativos. Os resultados foram apresentados em duas categorias temáticas: 1) A R/E como elemento que perpassa situações vividas no trabalho; 2) A R/E como uma dimensão presente na vida de pacientes e familiares. Evidenciou-se que, embora os profissionais da oncologia pediátrica considerem a R/E como uma dimensão importante no cuidado, a mesma ainda é compreendida como um recurso empregado sobretudo por pacientes e familiares, predominando, entre os profissionais, um sentido mais ligado a um protocolo do que a um efetivo recurso para o trabalho na área.
Palavras-chave: profissionais de saúde; neoplasias; criança; adolescente; espiritualidade
La inclusión de la religiosidad-espiritualidad (R-E) como una dimensión del cuidado de la salud aún plantea reflexiones, especialmente cuando analizamos las prácticas profesionales. Así, esta revisión integradora de la literatura tuvo como objetivo analizar cómo los profesionales de la oncología pediátrica experimentan la R/E en sus prácticas. A través de las bases/bibliotecas CINAHL, PsycINFO, Pubmed, SciELO y Lilacs se recuperaron 12 estudios producidos entre 2009 y 2019, nueve cualitativos y tres cuantitativos. Los resultados se presentaron en dos categorías temáticas: 1) R/E como elemento que permea las situaciones vividas en el trabajo; 2) la R/E como dimensión presente en la vida de los pacientes y familiares. Se evidenció que, si bien los profesionales de oncología pediátrica consideran a la R/E como una dimensión importante en el cuidado, se sigue entendiendo como un recurso utilizado principalmente por los pacientes y familiares, con predominio, entre los profesionales, de un sentido más ligado a un protocolo que un recurso eficaz para trabajar en el área.
Palabras clave: personal de la salud; neoplasias; niño; adolescente; espiritualidad
Cancer in children and adolescents is characterized as a global public health problem (Siegel et al., 2022), with impacts on morbidity and mortality, interfering in the lives of subjects, in health systems and demanding resources to meet emerging needs. Each year, 400,000 children and adolescents aged 0 to 19 years-old are diagnosed (World Health Organization (WHO), 2021), demonstrating that this disease is a complex problem that needs to be highlighted (Rossato et al., 2021).
The incidence of childhood cancer has grown in the last decade worldwide and is currently the leading cause of death from disease among children in Western countries (Barrios et al., 2022). In terms of mortality for year 2020, the International Agency for Research on Cancer estimated 107,833 deaths from cancer in childhood and adolescence, 61,689 for males and 46,144 for females (International Agency for Research on Cancer, 2022).
For the health team working in pediatric oncology, cancer in childhood and adolescence is characterized by being a complex situation that can affect the emotional conditions, being this one a difficult and avoided area, especially for those who have difficulty dealing with the possibility of death (Silva et al., 2019). The physical changes experienced by children/adolescents, painful and invasive procedures, changes in family relationships, the different responses to treatments, the limitations imposed by the disease, the possibility of death, situations of mourning, among other aspects, make the practice in pediatric oncology a perennial challenge.
Health professionals working in pediatric oncology need to constantly deal with demands that emerge in the health care process that require physical effort, technical capacity and emotional resources to face challenging situations in work practices (Alves, 2012). This way, facing adverse situations will require efforts of different natures and diversified strategies, one of which is religiosity/spirituality (R/S).
The inclusion of spirituality in the definition of health by the World Health Organization in 1998 (WHO, 1998) stimulated the number of studies whose object of study is aimed at understanding the effects of this dimension on the population’s living conditions. This way, religiosity and spirituality have gained space in care practices and have been described in the scientific literature as important elements in the health field because they interfere with the quality of life and the adopted coping conditions (Panzini et al., 2017; Pratiwi et al., 2018). In order to enable a broader discussion of these elements in this review, the combined term religiosity/spirituality (R/S) will be used, given that the epistemological distances between these terms do not always produce significant differences when we seek to understand health outcomes and, in this case, professional practices (Cunha & Scorsolini-Comin, 2020).
This dimension constantly permeates the experiences of cancer illness of adolescent and children and can positively or negatively affect how the patient and its family caregivers will deal with this process (Sposito et al., 2015; Walubita et al., 2018). Likewise, health professionals who deal with this population can also be affected by R/S because they are in contact with people who profess religious and spiritual beliefs and because this dimension is part of their subjectivity and sociocultural aspects.
What is discussed is that, paradoxically, R/S can either be an ally or hinder the work of these professionals in oncology care, since, because of being a sociocultural element; it influences the understanding of life and decision-making. In professional practices, what is observed is that these cultural elements that are present in life affect patients’ attitudes towards medical care and the ability to understand, manage and deal with the course of a disease, the meaning of a diagnosis and the consequences of the disease (Otmani & Khattab, 2018). Consequently, this will have an impact on the work carried out by the health team.
Although pediatric oncology care is a field with vast evidence and that R/S has gained emphasis in recent decades as a dimension that needs to be incorporated into health practices, it is noted that spiritual care is circumscribed and focused, in most cases, to the recipients of this care, that is, to children, adolescents and their family caregivers. Although the important role of the multidisciplinary team in this area is recognized, a substantially smaller production has been dedicated to understanding and valuing the importance and the meanings of R/S for the different professional categories.
It is important to understand how the scientific literature has described the ways in which R/S has permeated professional practices in the context of pediatric oncology, understanding this dimension as a resource and as a gap that hinders professional practice in this field of chronic and complex care represented by childhood cancer. Thus, the objective of this study was to understand how R/S has been evoked in the experiences of health professionals who work in pediatric oncology, based on the narratives produced by these protagonists in oncological care.
Materials and Method
This is an integrative review of the scientific literature carried out from January 1, 2009 to December 31, 2019. The following steps were carried out: (a) identification of the research problem; (b) literature search; (c) evaluation of studies; (d) data analysis; (e) interpretation (Hopia et al., 2016; Whittemore & Knafl, 2005).
The review considered the recommendations established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyse Protocols ((PRISMA); Moher et al., 2010) for performing searches, analysis and systematic description. The question that guided this study was developed through the PICO strategy, often considered in the reviews that are based on evidence-based practice, such as that of an integrative nature. The question to be answered from the review received the following wording: How has the scientific literature evidenced R/S in the experiences of health professionals in pediatric oncology?
Data collection was carried out in the databases/libraries Scientific Electronic Library Online (SciELO), Latin American and Caribbean Health Sciences Literature (Lilacs), Cumulative Index to Nursing and Allied Health Literature (CINAHL), National Library of Medicine of the USA (Pubmed) and Psychology Information (PsycINFO). Such databases/libraries were defined based on the literature that was intended to be collated, notably that of the field of health sciences and as they encompass scientific productions at an international and regional level (Latin America and the Caribbean). Thus, it was expected that the results would show how the scientific literature has approached this topic at a global level, but also in the social context in which the authors develop the research. The search criteria adopted considered the objectives of the review and descriptors that could evidence the state of scientific production on the target theme.
The keywords used and their combinations were: religiosity OR religion OR spirituality OR spiritual OR faith AND health personnel OR pediatric oncologist OR pediatric oncologists OR pediatric oncology OR oncologists OR oncologist AND neoplasms OR childhood cancer OR child with cancer OR adolescent with cancer and their respective terms in English and Spanish. In the Pubmed and PsycINFO databases, the keywords used were inserted only in English, given that they do not accept Portuguese at the time of the search.
As inclusion criteria, the following were selected: articles published within 10 years (January 2009-December 2019), written in English, Portuguese or Spanish, that focused on R/S in the work of health professionals and in personal experiences and that were fully available. The attention in pediatric oncology considered in the present review encompassed the different professional categories. Productions that were not articles (such as thesis, dissertations, chapters and books, for example), articles that escaped the theme, that had a population other than health professionals as a basis, repeated, in languages other than Portuguese, English and Spanish theoretical articles and the ones not found in full were excluded. The time period adopted sought to encompass the most recent productions found at the time the article was produced. It has been usual for reviews to adopt a period of 10 years in data retrieval, due to covering an adequate number of studies and current ones on the investigated themes.
For the discussion of the results, chaplains and religious/spiritual advisors were considered as members of the health team in this review for the work they develop with patients, family caregivers and other professionals who work in the context of child and adolescent cancer care. It is known that, in many situations, chaplains are considered spiritual professionals in the hospital environment, helping in decision-making, pain control, in the resolution of bioethical conflicts, in moments of patients’ spiritual crisis, among other aspects (Choi et al., 2015).
After carrying out the searches, the results were entered into the Rayyan Software (Ouzzani et al., 2016) for systematic organization and selection. The analysis of the evidence was carried out by two independent judges with experience with the subject and the disagreements analyzed and resolved by a third judge. The information collected was previously defined by two of the authors considering the objectives of the study and the PRISMA checklist and a standardized form were established to enter the information of the selected articles.
In order to answer the guiding question, the ways in which health professionals experienced R/S in cancer illness were presented and discussed in two categories produced later, that is, after reading and analyzing the material collected.
Results
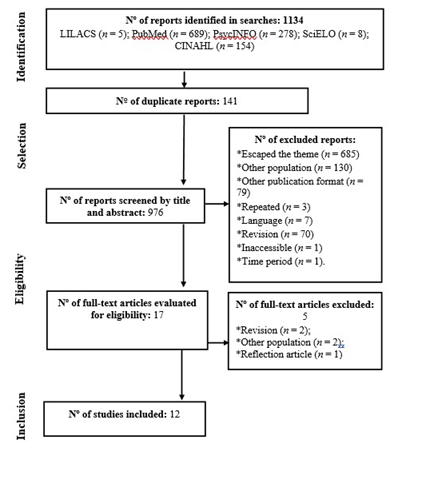
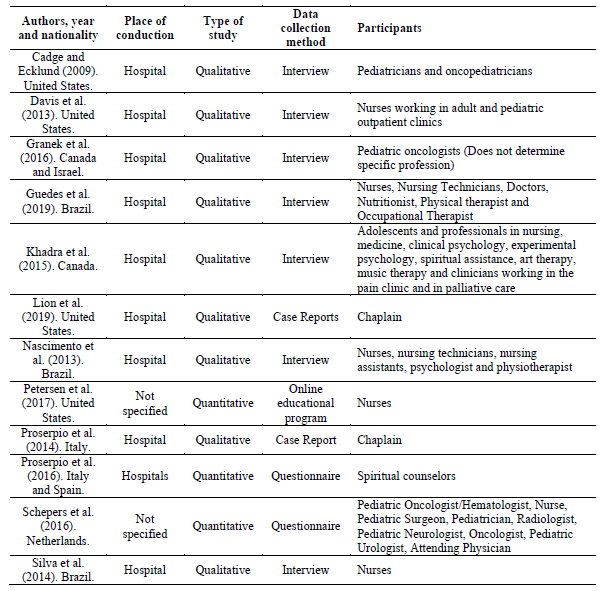
Figure 1 presents the flowchart of the process of selection of articles that were included in the study. After selecting and filtering the material, the final sample consisted of 12 articles, nine of which were qualitative and three were quantitative. Table 1 shows the articles in the final sample, authorship, year of production, nationality of authors, place of study, type of study, data collection method used and participants. After the final selection, the full reading was carried out to select the contents that would answer the guiding question.
Table 1: Articles according to authorship, year and nationality of authors, place of study, type of study and data collection method used
From the analysis of the contents of these articles that made up the corpus, two thematic categories were produced for data presentation: 1) R/S as an element that permeates situations experienced at work; 2) R/S as a dimension present in the lives of patients and families. The categories were created after analyzing all the material and focusing on the objectives of the study and synthesizing the main results observed. This way, the results that stood out the most and were similar were grouped, summarizing the two categories described here.
R/S as an element that permeates situations experienced at work
In this category, studies such as the one by Guedes et al. (2019) describe spirituality as one of the most used coping strategies by professionals participating in the research. According to the authors, spirituality was mentioned as a device that generates meaning in situations experienced, allowing the creation of meanings, which transcend life. In this study, R/S was also presented as a coping strategy that helps to deal with thoughts, with the palliative care provided and with the death of patients. It can be seen that the religious and personal beliefs of the professionals also justified the fact that they were working with children and adolescents with cancer based on notions such as purpose and mission.
A similar study was presented by Davis et al. (2013) about burnout in nurses’ work. The authors describe that R/S, along with the support of other co-workers, was one of the coping mechanisms used to deal with the stress arising from professional practices. According to the authors, such aspects can be understandable, since R/S is a dimension linked to personal transcendence, something that gives meaning to life, especially when these professionals need to deal with patients’ death situations.
R/S has been described as a resource to deal with the death of children and adolescents with cancer and with grieving circumstances. This aspect can be observed in the study by Granek et al. (2016) when describing that, although pediatric oncologists may not be religious, they still use faith and spirituality when they need to deal with a patient’s death. Still according to the authors, some professionals mention that death is not the “final stop”; there is a life beyond that. The professionals also had the belief that the child’s suffering had not been in vain, that there was a greater purpose in everything they lived through and that some upper force would take care of them after their departure (Granek et al., 2016).
Religion and faith were also mentioned as ways of dealing with the child’s death process in Silva et al. (2014). The authors describe that this dimension can comfort, reduce anguish and neutralize the stress experienced by professionals. In this study, the participants demonstrate the belief that the child’s death did not represent an absolute end, believing that there was something beyond materiality, a better place after death.
R/S was also questioned by health professionals. Guedes et al. (2019) present questions from the participants related to the motivations for God to have made the child/adolescent to get sick. However, these same participants saw illness as having a meaning for the existence of the child/adolescent in the material world, as if what they lived was determined by this upper force and there was a purpose for this. Still in relation to the studies found that observed R/S as an element of professional practice, Petersen et al. (2017) presents a skills and competence training program for nurses to develop the ability to work on aspects of R/S with their patients, observing these dimensions as important components in care practices.
Among the articles retrieved in the review, there is also evidence that religious and spiritual care is not always available in child and adolescent cancer treatment services. Proserpio et al. (2016) investigated the availability of spiritual support in pediatric oncology treatment centers in Italy and Spain, the role of spiritual counselors in these institutions and the training they had to deal with these aspects. The spiritual support service was available in 24 of the 26 treatment centers in Italy (92.3 %) and in 34 of the 36 in Spain (94.4 %). As for the role of the spiritual counselor, it usually involved providing religious services such as celebrating rites and administering the sacraments, providing end-of-life spiritual support, talking to families, and talking to teenagers.
The approach of R/S during the service provided or not addressing these aspects was also discussed by Cadge and Ecklund (2009). According to this study, there are situations in which there is no open dialogue with the patient or family about religious/spiritual issues, and professionals may limit themselves to considering specific aspects, such as cases in which the R/S of patients go against procedures that could be adopted. On the other hand, other professionals talk to their patients about these aspects, seeking to offer something that goes beyond traditional care, especially in cases where there is no longer any possibility of curing the disease.
Cadge and Ecklund (2009) found that pediatric oncologists are more likely than pediatricians to see patients’ R/S as relevant to their practices and, when they talk about these aspects, they are able to establish more permeable boundaries between religion, spirituality and medicine. However, there are cases in which R/S is seen as a barrier that prevents the work and/or the care provided, especially in more traditional or orthodox religious denominations that manifest dogmas that conflict with biomedical aspects of care.
R/S as a dimension present in the lives of patients and families
In this category, a study by Cadge and Ecklund (2009) shows that the number of physicians aware that R/S helps patients and families to face the process of becoming ill has increased, especially in cases of life-threatening diseases, as is the case of cancer. Comprehensive care for the patient’s needs, including spiritual care, was described by Nascimento et al. (2013) as a factor that interferes in the improvement of the patient’s quality of life and also in the performance of a good job by the multiprofessional team. Still in this sense, Schepers et al. (2016) showed that health professionals consider R/S important for the family, but consider it less than family caregivers.
Proserpio et al. (2014), when investigating the activities developed by the chaplain in a hospital in Milan, described that the work of this professional was associated with offering spiritual support for people to deal with questions and aspects of experiences with R/S. In the descriptions made by these authors, it is still possible to observe that the chaplain’s work was also developed through counseling to patients, establishing contact with the religious institution of the sick person to resume bonds, dialogues regarding the doubts they had about their own R/S when they questioned whether God had abandoned them and the acceptance of existential questions. The reception provided by the chaplain to the parents took place by answering prayer requests, holding conversations about the fear of death or about conflicts that arose between the two parents.
The chaplain’s welcoming of family members was also described in the study by Lion et al. (2019). In this study, it is possible to observe that the chaplain often ends up welcoming the families in relation to several aspects that emerge, such as in situations of stress, fear, anxiety, anticipatory grief, frustrations, questions, mental illness, about the meanings of faith in the disease, among other aspects. Another way in which R/S was present in the assistance provided by chaplains was when they prayed for people undergoing treatment and also for professionals with the aim of comforting, showing mercy, thanksgiving and wisdom for decision-making, for healing, among others.
Cadge and Ecklund (2009) also describe that health professionals perceive R/S as an element present in the lives of family members, especially when they need to make difficult decisions or when patients are dying. This study also describes that the R/S of patients and family members can be an aspect that interferes with the provision of care in situations where there are conflicts between religious/spiritual beliefs and procedures to be performed.
The experiences of R/S in pediatric oncology are not always completely positive. Study carried out by Khadra et al. (2015), with the objective of developing a suffering scale for adolescents with cancer, highlighted existential and religious suffering in interviews with oncology professionals and patients.
Regarding the professionals’ perception of the interference of R/S in the care provided, Cadge and Ecklund (2009) emphasize that in certain situations there may be tensions between people’s beliefs and the necessary procedures to be developed due to illness. According to the authors, people’s R/S can influence decision-making, lead them to have a notion of knowledge that is different from medical knowledge, interfering in dimensions such as acceptance of treatment and necessary procedures from a medical point of view. In some of these situations, the authors describe that the professionals respect the decisions of the families until the moment that they can cause a compromise in the health/life of the patients, prioritizing the maintenance of children’s lives, despite the parents’ choices.
Discussion
The present review has shown a gap in the production of scientific knowledge regarding the study of religious and spiritual aspects in the personal and professional experiences of the pediatric oncology health team. During the selection of material, it was observed that there is a significant number of publications that consider R/S in the practices of pediatric professionals. However, when the focus turns to pediatric oncology, the results are considerably restricted. In addition to this, in some cases, it is observed that R/S is approached tangentially, being only mentioned as a dimension that influences the lives of subjects, an important resource for coping with personal and work situations or as a component of comprehensive health care, without it being possible to analyze it in more detail.
Based on this finding, it can be questioned that R/S, even if it is scientifically recognized and as an index encompassed by evidence-based practices, ends up being compared as a dimension of lesser value when we analyze the experiences of these professionals. As a resource, it is thus shown to be underused or under investigated. Added to this, R/S is more mentioned in studies with patients and their families, as if this were a powerful resource in coping with cancer and not in the development of a more humanized and reflective care by health professionals.
Another aspect that deserves attention in relation to the scientific production found refers to the fact that most publications do not focus on how health professionals are impacted by R/S in their personal experiences. That is, there is a significant portion of these studies that are aimed at describing how professionals perceive R/S in the lives of patients and family members, without describing in detail how R/S permeates personal experiences or how it interferes with their subjectivity and its emotional aspects (Cadge & Ecklund, 2009; Guedes et al., 2019; Lion et al., 2019).
This movement reveals that R/S is still a resource little explored in the experiences of these professionals, who have difficulty in positioning themselves in relation to their own R/S and the use of this dimension in care, in a possible effect of a biomedical tradition that emphasizes the search for neutrality and the distance between patient and professional (Cunha & Scorsolini-Comin, 2020). This difficulty of insertion of R/S on the part of professionals in the area may be based on the understanding spread by the biomedical model that science and spirituality are, in fact, irreconcilable, promoting the following paradox: R/S can be used by the patient, but not by the professional, as it is based on science (Dal-Farra & Geremia, 2010).
Thus, the meaning of the professionals’ R/S itself, the understanding of it as a facilitator in the face of stressful situations and that should be integrated into the practice of care (Arrieira et al., 2018) ends up not being embodied in practice or being understood as something that cannot be offered due to other care needs that are considered more priority in the interventions they carry out (Nascimento et al., 2016). In practice, neutrality positions tend to operate in the sense that R/S is a dimension that can be evoked and developed only by those who receive care, which can promote a fragmented and inauthentic health practice precisely because of non-involvement of the professionals in this field. This aspect can promote what Neubern (2013) calls unwelcoming reception, with important repercussions for the humanization of care.
When analyzing the studies, the need to consider chaplaincy professionals as team members was perceived, even without necessarily having an academic background in health courses. These professionals have been included as an important category for the care provided, mainly due to the fact that R/S has gained more space to be considered in the contexts of people’s illness. The chaplains often have a religious/spiritual training/path from different religious denominations and in care contexts they work in an integrated way with multidisciplinary teams and health facilities, being considered as members of the care process provided to patients, family members and to other team members who work in the services (Lion et al., 2019; Proserpio et al., 2016).
Among the study participants, medical and nursing professionals stand out as being the ones that were most evident. This data reflects an aspect that is remarkable in the contexts of child and adolescent cancer care, as these two professional categories end up being the ones that have the most contact with patients and family members. This finding can be justified by considering that nurses, for example, are the largest group in the health system and provide full-time care, being more likely to find patients with spiritual needs (Chiang et al., 2016) and, therefore, studies focusing on these professionals can be prioritized.
Regarding the ways in which R/S is described in the personal and professional experiences of the pediatric oncology health team, it is clear that the subsidies offered by this dimension are important to be considered, as this work environment is demarcated for being potentially stressor. Faced with the suffering condition of the patient and their families, the health team ends up expressing feelings and emotions such as pity, compassion and love, guilt and anxiety, anger and hurt (Oliveira & Firmes, 2012). In this way, R/S can be a support mechanism for the conditions they experience in work practices.
R/S can also be important for health professionals when they realize that this dimension can be a complementary therapy to treatment. A study by Sampaio and Siqueira (2016) showed, for example, that nurses recognize R/S as an element that influences the way patients will experience conditions of suffering, recovery, and the meaning of life. King et al. (2013), when investigating the perception of physicians about the R/S of patients in pediatric and oncology environments, showed that these professionals believe that this dimension is relevant because it provides a support system in times of crisis, has repercussions on behaviors and decisions related to health, positively affect health and help in the therapeutic relationship between the professional, the patient and the family.
R/S was also observed when health professionals needed to deal with situations that involved the possibility of death or death of patients. It is observed that R/S supports them in a delicate moment of being faced and created conditions for them to believe that death would not be the final limit of existence. Silva Junior et al. (2016), when describing the use of R/S in oncology, mention that professionals perceive the process of death contained in their personal religious conceptions, defining it on some occasions as a passage, leading to the symbolic representation of a path to well-being and relief from suffering. However, it is important to emphasize that it should not be considered as a resource to be used only at the time of the patient’s death or when there is no other alternative for treatment, as it is present throughout people’s development and not only at the end of life.
Another aspect worth mentioning is that, during the selection of articles that would enter the sample, it was possible to observe an association between R/S, palliative care and people hospitalized in the Intensive Care Unit (ICU). This aspect raised questions about the emphasis that is given to R/S in these phases of treatment and why investigations specifically focus on these moments. These questions are in line with the data presented by Choi et al. (2015), when they describe that most meetings of patients with chaplains occur in the last day or two of life, meaning that visits to chaplains are usually requested for patients who are actively dying, and not with the aim of proactive spiritual support for families and patients. Chaplain involvement in the ICU is also not frequent, but appears to become more frequent in critically ill patients, and becomes the norm for dying patients (Choi et al., 2015). That is, R/S seems to be used more at the time of death than during the entire illness process.
In the articles selected, R/S was considered by health professionals as an element of care provided to family caregivers and that provided conditions for coping with all stages of child and adolescent cancer care. A review study published by Robert et al. (2019) analyzing the importance of spiritual care in pediatric oncology shows that spiritual support is a supportive and useful resource for patients and family caregivers in coping with the disease.
The interferences of the R/S of family members in professional practices were also evidenced and are important to be considered. It is known that in certain situations people’s beliefs conflict with procedures that need to be performed, leading to complex bioethical conflicts. These emerging bioethical conflicts remind us that not every relationship between spirituality/religion/religiosity and health is balanced, and it is evident that in the processes that involve dialogue between these fields, confrontation and discussion arise in the face of existential issues (Tavares et al., 2016).
Final Remarks
The review presented here evidenced the scarcity of scientific productions that focus on the influence of R/S in the work and personal experiences of pediatric oncology professionals. The results presented indicate that there is a difference in the way R/S is described in the experiences of patients and family members in relation to how it is presented in the daily lives of health professionals. When used by patients and family members, this dimension is described as a resource in facing the difficult situations that are experienced in the diagnosis, the treatment course, cure or end of life. However, when evidenced and related to health professionals, it becomes another protocol to be followed, it focuses on the perception of the health team in relation to the R/S of the sick person and its caregiver, without actually being seen as a potential and experiential resource that could provide reception and support for the practices they develop and which are difficult to face.
The data revealed that health professionals have considered R/S in their practices and its importance has gained more emphasis over the years, with the search for comprehensive care through the actions developed. Nursing and medical professionals are the most mentioned when dealing with the R/S aspects of sick children/adolescents. The chaplaincy, on the other hand, stood out as part of the care team for people that are sick with cancer and has offered some of the main care related to the religious and spiritual aspects that emerge in this context.
The bioethical conflicts related to R/S that permeate work practices in pediatric oncology showed a relevant component that can emerge as a result of the opposition between people’s beliefs and the methods that are to be used in health care. This data showed that there will not always be a friendly and harmonious relationship between R/S and health practices, so that the work of several professionals from different backgrounds will be important in conducting dialogues between the sick person, his or her family and the health team.
The implications for practice reinforce the need to evoke with these professionals their own experiences in relation to R/S, as well as this element can emerge in their practices. It is necessary that empirical studies focus on the production of this evidence, which can be useful both for promoting a more comprehensive and humanized care and for a better understanding of the Intersubjective aspects of these professionals. The results found demonstrate the need to consider R/S in health contexts, as this dimension is present in the lives of patients, family members, and the health team and can help in the experiences of illness or being a factor that will be challenging for the patient care provided when it causes conflicts between people’s beliefs and the procedures that will need to be developed. All of these elements converge so that R/S is a component to be incorporated into the training curricula of the different professions in the health area that may have to deal with this dimension in the professional practices they develop, such as care in pediatric oncology.
As limitations of this study, the fact that the studies, although aiming to investigate R/S in health professionals, end up focusing on how they observe this dimension in patients or family members is evidenced. Thus, the results show only a little of how R/S is experienced by these professionals in their personal lives or how it can interfere, for example, with subjectivity and mental health conditions and, consequently, with how they deal with aspects of the work context, especially those who mobilize feelings in relation to what is experienced. It is also observed that there are few studies in the national reality whose objective was to investigate R/S specifically in pediatric oncology. Thus, it is relevant that further investigations be carried out, mainly with a focus on understanding how R/S can be a coping resource and its implications/associations with levels of mental health in this population.
REFERENCES
Alves, R. (2012). Vivências de profissionais de saúde na assistência a crianças e adolescentes com câncer: Um estudo fenomenológico (Dissertação de Mestrado, Universidade de São Paulo). https://www.ffclrp.usp.br/imagens_defesas/17_12_2012__10_48_45__61.pdf [ Links ]
Arrieira, I. C. D. O., Thofehrn, M. B., Porto, A. R., Moura, P. M. M., Martins, C. L., & Jacondino, M. B. (2018). Espiritualidade nos cuidados paliativos: Experiência vivida de uma equipe interdisciplinar. Revista da Escola de Enfermagem da USP, 52, e03312. https://dx.doi.org/10.1590/s1980-220x2017007403312 [ Links ]
Barrios, P., Enesco, I., & Varea, E. (2022). Emotional experience and type of communication in oncological children and their mothers: hearing their testimonies through interviews. Frontiers in Psychology, 13, 834312. https://doi.org/10.3389/fpsyg.2022.834312 [ Links ]
Cadge, W. & Ecklund, E. H. (2009). Prayers in the clinic: How pediatric physicians respond. Southern Medical Journal, 102(12), 1218-1221. https://doi.org/10.1097/SMJ.0b013e3181bfac71 [ Links ]
Chiang, Y. C., Lee, H. C., Chu, T. L., Han, C. Y., & Hsiao, Y. C. (2016). The impact of nurses' spiritual health on their attitudes toward spiritual care, professional commitment, and caring. Nursing Outlook, 64(3), 215-224. https://doi.org/10.1016/j.outlook.2015.11.012 [ Links ]
Choi, P. J., Curlin, F. A., & Cox, C. E. (2015). “The patient is dying, please call the chaplain”: The activities of chaplains in one medical center's intensive care units. Journal of Pain and Symptom Management, 50(4), 501-506. https://doi.org/10.1016/j.jpainsymman.2015.05.003 [ Links ]
Cunha, V. F. & Scorsolini-Comin, F. (2020). Brazilian psychotherapists and the dimension of religiosity/spirituality. Counselling and Psychotherapy Research, 20(4), 1-9. https://doi.org/10.1002/capr.12357 [ Links ]
Dal-Farra, R. A. & Geremia, C. (2010). Educação em saúde e espiritualidade: Proposições metodológicas. Revista Brasileira de Educação Médica, 34(4), 587-597. https://doi.org/10.1590/S0100-55022010000400015 [ Links ]
Davis, S., Lind, B. K., & Sorensen, C. (2013). A comparison of burnout among oncology nurses working in adult and pediatric inpatient and outpatient settings. Oncology Nursing Forum, 40(4), E303-E311. https://doi.org/10.1188/13.ONF.E303-E311 [ Links ]
Granek, L., Barrera, M., Scheinemann, K., & Bartels, U. (2016). Pediatric oncologists' coping strategies for dealing with patient death. Journal of Psychosocial Oncology, 34(1-2), 39-59. https://doi.org/10.1080/07347332.2015.1127306 [ Links ]
Guedes, A. K. C., Pedrosa, A. P. A., Osório, M. O., & Pedrosa, T. F. (2019). Cuidados paliativos em oncologia pediátrica: Perspectivas de profissionais de saúde. Revista da SBPH, 22(2), 128-148. [ Links ]
Hopia, H., Latvala, E., & Liimatainen, L. (2016). Reviewing the methodology of an integrative review. Scandinavian Journal of Caring Sciences, 30(4), 662-669. https://doi.org/10.1111/scs.12327 [ Links ]
International Agency for Research on Cancer. (2022). Cancer today. https://gco.iarc.fr/ [ Links ]
Khadra, C., Le May, S., Tremblay, I., Dupuis, F., Cara, C., Mercier, G., Vachon, M. F., & Lachance Fiola, J. (2015). Development of the adolescent cancer suffering scale. Pain Research and Management, 20(4), 213-219. https://doi.org/10.1155/2015/645367 [ Links ]
King, S. D., Dimmers, M. A., Langer, S., & Murphy, P. E. (2013). Doctors' attentiveness to the spirituality/religion of their patients in pediatric and oncology settings in the Northwest USA. Journal of Health Care Chaplaincy, 19(4), 140-164. https://doi.org/10.1080/08854726.2013.829692 [ Links ]
Lion, A. H., Skiles, J. L., Watson, B. N., Young, J. D., & Torke, A. M. (2019). Chaplain care in pediatric oncology: Insight for interprofessional collaboration. Pediatric Blood & Cancer, 66(12), e27971. https://doi.org/10.1002/pbc.27971 [ Links ]
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Prisma Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097 [ Links ]
Nascimento, D. M., Rodrigues, T. G., Soares, M. R., Rosa, M. L. S., Viegas, S. M. D. F., & Salgado, P. D. O. (2013). Experiência em cuidados paliativos à criança portadora de leucemia: A visão dos profissionais. Ciência & Saúde Coletiva, 18, 2721-2728. [ Links ]
Nascimento, L. C., Oliveira, F. C. S. D., Santos, T. D. F. M., Pan, R., Santos, M. F., Alvarenga, W. A., & Rocha, S. M. M. (2016). Atenção às necessidades espirituais na prática clínica de enfermeiros. Aquichan, 16(2), 179-192. https://doi.org/10.5294/aqui.2016.16.2.6 [ Links ]
Neubern, M. (2013). Psicoterapia e espiritualidade. Diamante. [ Links ]
Oliveira, M. C. L. D. & Firmes, M. D. P. R. (2012). Sentimentos dos profissionais de enfermagem em relação ao paciente oncológico. Revista Mineira de Enfermagem, 91-97. [ Links ]
Organização Mundial da Saúde. (1998). Division of mental health and prevention of substance abuse. WHOQOL and spirituality, religiousness and personal beliefs (SRPB). [ Links ]
WHO. (2021). Childhood Cancer. https://www.who.int/news-room/fact-sheets/detail/cancer-in-children [ Links ]
Otmani, N. & Khattab, M. (2018). Informational support in pediatric oncology: review of the challenges among Arab families. Journal of Cancer Education, 33(4), 732-736. https://doi.org/10.1007/s13187-016-1137-8 [ Links ]
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan - A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4 [ Links ]
Panzini, R. G., Mosqueiro, B. P., Zimpel, R. R., Bandeira, D. R., Rocha, N. S., & Fleck, M. P. (2017). Quality-of-life and spirituality. International Review of Psychiatry, 29(3), 263-282. https://doi.org/10.1080/09540261.2017.1285553 [ Links ]
Petersen, C. L., Callahan, M. F., McCarthy, D. O., Hughes, R. G., White-Traut, R., & Bansal, N. K. (2017). An online educational program improves pediatric oncology Nurses’ knowledge, attitudes, and spiritual care competence. Journal of Pediatric Oncology Nursing, 34(2), 130-139. https://doi.org/10.1177%2F1043454216646542 [ Links ]
Pratiwi, E., Mulatsih, S., & Setiyarini, S. (2018). Spirituality relationship to the quality of life of children with cancer in Dr. Sardjito General Hospital. International Journal of Community Medicine and Public Health, 5(3), 880-884. http://dx.doi.org/10.18203/2394-6040.ijcmph20180741 [ Links ]
Proserpio, T., Ferrari, A., Veneroni, L., Giacon, B., Massimino, M., & Clerici, C. A. (2014). Spiritual aspects of care for adolescents with cancer. Tumori Journal, 100(4), 130-135. https://doi.org/10.1700%2F1636.17926 [ Links ]
Proserpio, T., Veneroni, L., Silva, M., Lassaletta, A., Lorenzo, R., Magni, C., Bertolotti, M., Barisone, E., Mascarin, M., Jankovic, M., D'Angelo, P., Clerici, C. A., Garrido-Colino, C., Gutierrez-Carrasco, I., Echebarria, A., Biondi, A., Massimino, M., Casale, F., Tamburini, A., & Ferrari, A. (2016). Spiritual support for adolescent cancer patients: A survey of pediatric oncology centers in Italy and Spain. Tumori Journal, 102(4), 376-380. https://doi.org/10.5301%2Ftj.5000494 [ Links ]
Robert, R., Stavinoha, P., Jones, B. L., Robinson, J., Larson, K., Hicklen, R., Smith, B., Perko, K., Koch, K., Findley, S., & Weaver, M. S. (2019). Spiritual assessment and spiritual care offerings as a standard of care in pediatric oncology: A recommendation informed by a systematic review of the literature. Pediatric Blood & Cancer, 66(9), e27764. https://doi.org/10.1002/pbc.27764 [ Links ]
Rossato, L., Benfato, J. C., Ullán, A. M., & Scorsolini-Comin, F. (2021). Religious-spiritual experiences of family members and caregivers of children and adolescents with cancer. Palliative & Supportive Care, 1-9. https://doi.org/10.1017/S1478951521001590 [ Links ]
Sampaio, A. D. & Siqueira, H. C. H. (2016). Influência da espiritualidade no tratamento do usuário oncológico: Olhar da enfermagem. Ensaios e Ciência: Ciências Biológicas, Agrárias e da Saúde, 20(3), 151-158. [ Links ]
Schepers, S. A., Haverman, L., Zadeh, S., Grootenhuis, M. A., & Wiener, L. (2016). Healthcare professionals’ preferences and perceived barriers for routine assessment of patient‐reported outcomes in pediatric oncology practice: moving toward international processes of change. Pediatric Blood & Cancer, 63(12), 2181-2188. https://doi.org/10.1002/pbc.26135 [ Links ]
Siegel, R. L., Miller, K. D., Fuchs, H. E., & Jemal, A. (2022). Cancer statistics, 2022. CA: A Cancer Journal for Clinicians, 72(1), 7-33. https://doi.org/10.3322/caac.21708 [ Links ]
Silva Junior, R. F., Lima, K. U., Eugênio, K. K., Gomes, N. T., de Carvalho, P. D., & Silva, F. W. S. (2016). Refletindo sobre a espiritualidade e a religiosidade relacionadas à prática dos profissionais de saúde na oncologia. Revista Eletrônica Acervo Saúde, (4), S178-S185. [ Links ]
Silva, M. M., Vidal, J. M., Leite, J. L., & Silva, T. P. (2014). Estratégias de cuidados adotadas por enfermeiros na atenção à criança hospitalizada com câncer avançado e no cuidado de si. Ciência, Cuidado e Saúde, 13(3), 471-478. https://doi.org/10.4025/cienccuidsaude.v13i3.19937 [ Links ]
Silva, S., Melo, C. F., & Magalhães, B. (2019). A recidiva em oncologia pediátrica a partir da perspectiva dos profissionais. Psicologia, Saúde & Doenças, 20(2), 542-555. https://dx.doi.org/10.15309/19psd200221 [ Links ]
Sposito, A. M. P., Silva‐Rodrigues, F. M., Sparapani, V. D. C., Pfeifer, L. I., Lima, R. A. G., & Nascimento, L. C. (2015). Coping strategies used by hospitalized children with cancer undergoing chemotherapy. Journal of Nursing Scholarship, 47(2), 143-151. https://doi.org/10.1111/jnu.12126 [ Links ]
Tavares, C. Q., Valente, T. C., Cavalcanti, A. P. R., & Carmos, H. O. (2016). Espiritualidade, religiosidade e saúde: Velhos debates, novas perspectivas. Interações, 11(20), 85-97. https://doi.org/10.5752/P.1983-2478.2016v11n20p85 [ Links ]
Walubita, M., Sikateyo, B., & Zulu, J. M. (2018). Challenges for health care providers, parents and patients who face a childhood cancer diagnosis in Zambia. BMC Health Services Research, 18(1), 314. https://doi.org/10.1186/s12913-018-3127-5 [ Links ]
Whittemore, R. & Knafl, K. (2005). The integrative review: updated methodology. Journal of Advanced Nursing, 52(5), 546-553. https://doi.org/10.1111/j.1365-2648.2005.03621.x [ Links ]
World Health Organization. (1998). Division of mental health and prevention of substance abuse. WHOQOL and spirituality, religiousness and personal beliefs (SRPB) [ Links ]
World Health Organization. (2021). Childhood Cancer. https://www.who.int/news-room/fact-sheets/detail/cancer-in-children [ Links ]
Funding: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior ((CAPES), Coordination for the Improvement of Higher Education Personnel).
How to cite: Rossato, L., Salgado Sena, B. T, Nascimento, L. C., & Scorsolini-Comin, F. (2022). Religiosity/spirituality (R/S) in professional practice in pediatric oncology: resource or protocol? Ciencias Psicológicas, 16(2), e-2324. https://doi.org/10.22235/cp.v16i2.2324
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. L. R. has contributed in a, b, c, d, e; B. T. S. S. in a, b, c, d, e; L. C. N. in a, c, d, e; F. S-C. in a, c, d, e.
Received: October 17, 2020; Accepted: October 21, 2022











 texto en
texto en