Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Ciencias Psicológicas
versión impresa ISSN 1688-4094versión On-line ISSN 1688-4221
Cienc. Psicol. vol.16 no.2 Montevideo dic. 2022 Epub 01-Dic-2022
https://doi.org/10.22235/cp.v16i2.2250
Original Articles
Adaptation for online implementation of a Positive Psychology intervention for health promotion
1 Universidade Federal de Pelotas, Brasil, helen.durga@gmail.com
2 Universidade La Salle e Universidade Federal do Rio Grande do Sul, Brasil
This study describes the online adaptation of a Positive Psychology intervention for health promotion. The methodological guidelines used were The Formative Method for Adapting Psychotherapy and the Consolidated Framework for Implementation, based on: characteristics of the intervention; of the individuals; internal and external contexts; implementation process. The intervention consisted of 6 online group sessions, with 10 staff members from the health management team of a retiree association in RS/Brazil, mean age 43.6 years (SD = 15.86). An evaluation questionnaire was completed at the end of the activities and descriptive statistics revealed participants' satisfaction with the intervention and with the moderator, as well as generalization of the contents. Changes were suggested specially to increase the duration of the sessions. We suggest the systematization the processes used in this study to support research on the implementation and adaptation of online interventions for different contexts and populations.
Keywords: positive psychology; health promotion; online adaptation
Este estudo descreve a adaptação online de uma intervenção em Psicologia Positiva para promoção de saúde. Como diretriz metodológica, utilizou-se o The Formative Method for Adapting Psychotherapy e o Consolidated Framework for Implementation Research, nos eixos: características da intervenção; dos indivíduos; contextos interno e externo; processo de implementação. A intervenção consistiu em 6 encontros grupais online, com 10 integrantes da equipe de gestão em saúde de uma associação de aposentados do RS, Brasil, média de idade 43,6 anos (DP = 15,86). Um questionário de avaliação foi preenchido ao final das atividades e estatísticas descritivas revelaram satisfação dos participantes com a intervenção e com o moderador, assim como generalização dos conteúdos. Foram sugeridas alterações, especialmente aumento da carga horária das sessões. Sugere-se a sistematização dos processos utilizados neste estudo para embasar pesquisas de implementação e adaptação de intervenções online para diferentes contextos e público-alvo.
Palavras-chave: psicologia positiva; promoção de saúde; adaptação online
Este estudio describe la adaptación online de una intervención en Psicología Positiva para la promoción de la salud. Como guía metodológico se utilizó el The Formative Method for Adapting Psychotherapy y Consolidated Framework for Implementation Research en: características de la intervención; de individuos; contextos internos y externos; proceso de implementación. La intervención consistió en 6 reuniones grupales con 10 miembros del equipo de gestión de salud de una asociación de jubilados en RS (Brasil), con una edad promedio de 43.6 años (DE = 15.86). Se completó un cuestionario de evaluación al final de las actividades y las estadísticas descriptivas revelaron la satisfacción de los participantes con la intervención, con el moderador y generalización de los contenidos. Se sugirieron cambios, especialmente aumento en la carga de trabajo de las sesiones. Sugerimos sistematizar los procesos utilizados en este estudio para apoyar la investigación sobre la implementación y adaptación de intervenciones para diferentes contextos y públicos.
Palabras clave: psicología positiva; promoción de la salud; adaptación online
The year 2020 was a turning point in human history after the World Health Organization (WHO, 2020a, 2020b) announced a pandemic as a public health emergency. First detected in Wuhan, China, COVID-19 is a severe acute respiratory syndrome caused by the new Betacoronavirus 2 (SARS-CoV2), called new coronavirus (Huang et al., 2020; Spina et al., 2020). Besides the rapid progression to severe cases of the disease, another difference of COVID-19 vis-à-vis other infectious conditions is the high contagion rate between individuals/groups, or prolonged contagion after the exposure to virus-contaminated surfaces (Duan et al., 2020). Although the final death rates from COVID-19 cannot yet be ascertained due to the rapid progression of the disease in several countries, case fatality rates have been higher than previous crises of the 21st century caused by SARS-CoV and MERS-CoV coronaviruses. Currently, cases have been underreported due to the shortage of samples, reagents and equipment for testing and diagnostic establishment worldwide (Driggin et al., 2020; Watkins, 2020).
Concerning individuals’ mental and physical health due to the imminent risk of infection by the virus and physical distancing/isolation and break in the life routine, we highlight factors intervening in the pandemic that trigger uncertainty about the future and psychological crises. Moreover, there is a low perception of control and insecurity regarding the support provided by social institutions to mitigate socioeconomic problems arising from job losses, reduction or non-existence of jobs and income, in the case of informal workers, service providers, and companies. In addition, the lack of public policies and investments to meet the basic needs to face the pandemic is a stressor attaching risks to people’s mental health. We also witness a lack of managers’ preparedness and the inconsistent provision of information on safety procedures to the population by public authority levels and bodies, which tends to generate even more anxiogenic and depressogenic symptoms for the population and, mainly, those included in a risk group (WHO, 2020a, 2020b).
Health promotion and disease prevention strategies are the primary interventions suggested addressing such complex mental health issues. They serve to treat pre-clinical, underdiagnosed cases or clinical symptoms and prevent the recurrence of health problems and as a measure to compile evidence to guide and support the elaboration of public policies and sustainability of the health network (WHO, 2020a, 2020b).
Health promotion interventions have been implemented in several countries in online/virtual format (also called eHealth/mHealth interventions) for greater capillarity of access for risk groups due to their low cost (Welch et al., 2016) and because they are more effective for behavioral changes, given their interactive nature, when compared to motivational or purely informative websites (Mouton & Cloes, 2013).
Some examples of interventions implemented online to promote the health of adults and older adults are geared to informal caregivers (family members) that include professional and social support components, instructions for behavioral change, and problem-solving (Richard et al., 2019); cancer patients and their caregivers (Northouse et al., 2014); self-directed interventions for several mental health conditions (post-traumatic stress, depression, anxiety, and phobia) and physical health (diet and physical activity) (Rogers et al., 2017). Among the most significant benefits to mental health identified after participating in online interventions, review data indicate a lower depressive level in interventions by apps focused on health promotion than cognitive training apps (Firth et al., 2017) and gains in the prevention of depression (Ebert et al., 2017).
In Brazil, some regulations are also in force to regulate the work of psychologists through information and communication technologies (ICTs) for remote access of intervention participants, such as Resolution No. 11, of May 11, 2018, which regulates the provision of psychological services performed through ICTs. Resolution No. 11/2018 regulates the Psychological Assessment practice. Technical Note No. 07/2019 guides on the use of psychological tests in services performed through ICTs. Resolution Nº 04, of March 26, 2020, provides for the regulation of psychological services provided through ICTs during the COVID-19 pandemic and assists in the registration of psychologists for online services (Marasca et al., 2020).
Thus, at this time of grave need, it is impossible to act with group face-to-face interventions due to the restrictive measures in several countries to promote physical distance from the general population and contain COVID-19 transmission. Whereas there is no defined deadline for the normalization of standard procedures for assistance and provision of health services; whereas it is essential to adapt services and interventions for health promotion, based on the use of ICTs for distance/remote access. This study aims to describe the process of adapting an intervention in Positive Psychology for health promotion with online implementation Vem Ser Program.
Description of the intervention: The Vem Ser Program
Positive Psychological Interventions (PPIs) have been implemented worldwide to promote physical and mental health. This intervention model includes approaches to positive subjective experiences, traits that are strengths, which constitutes character virtues, and positive institutional contexts to favor better psychological and health functioning (Durgante, 2017; Magyar-Moe et al., 2015; Proyer et al., 2014; Sin & Lyubomirsky, 2009).
PPIs have been effective in improving well-being and quality of life indicators in clinically and non-clinically diagnosed individuals (Boiler et al., 2013; Durgante & Dell’Aglio, 2019; Nikrahan et al., 2016), providing better response to treatments and rehabilitation (Reppold et al., 2015), better recovery from adverse psychophysiological effects, such as cardiovascular reactivity, inflammatory processes, and immunosuppression, which tend to be aggravated in stressing situations (Cohn & Fredrickson, 2010).
Thus, the Vem Ser Program was developed based on the scientific literature on group PPIs (Sin & Lyubomirsky, 2009) and Cognitive-Behavioral Therapy (Knapp & Beck, 2008). The program consists of 6 weekly (2 h each) face-to-face group sessions and aims to intervene in the following forces: values and self-care/prudence, optimism, empathy, gratitude, forgiveness, the meaning of life, and work. The initial version of the program, implemented face-to-face, underwent a pilot study (Durgante et al., 2020a), a feasibility study (Durgante et al., 2019b), and an efficacy trial (Durgante & Dell’Aglio, 2019), with a sample of more than a hundred southern Brazilian retirees. Quantitative results indicated the main effects of the program for improved indicators of life satisfaction, resilience, symptoms of perceived stress, depression, and anxiety in the intervention group, besides interaction effects for improved optimism, empathy, symptoms of depression and anxiety in the experimental group compared to the control group. The effects and impacts on life satisfaction, depression, and anxiety symptoms remained three months after the end of the program (Durgante et al., 2020b). However, given the current pandemic situation and the need to adapt services remotely for all populations and health care levels, the online version of the program was adapted to conduct interventions aimed at the general public (Durgante et al., 2019a).
Methods
Design
A mixed qualitative-quantitative longitudinal study was developed to implement and evaluate the online version of the Vem Ser Program, with pre (T1- in the week before the onset of the intervention) and post-intervention (T2- in the week of the end of sessions). This was based on the Formative Method for Adapting Psychotherapy (Hwang, 2009), in five stages: I. Generating knowledge and collaboration with stakeholders; II. Integrating the information generated with theory and empirical and clinical knowledge; III. Reviewing and initiating the intervention in the adapted format with the stakeholders/target audience; IV. Conducting preliminary tests with the adapted version of the intervention; V. Finalizing the culturally adapted version of the intervention. We employed the Consolidated Framework for Implementation Research (CFIR) (Damschroder et al., 2009), as a methodological guideline used to consider the necessary adjustments/adequacies to adapt the intervention to the new health context/organization/institution and online format. It considers 29 criteria subdivided into the following assessment axes: intervention characteristics; internal and external contexts; characteristics of the individuals involved; implementation process. We evaluated quantitative data by descriptive statistics and qualitative data by the Thematic Content Analysis (Saldaña, 2009), with the axes and criteria established in the CFIR (Damschroder et al., 2009).
Participants
Ten health management team members of an association of retirees in the State of Rio Grande do Sul, Brazil, of which nine were females, participated by convenience and voluntarily. The sample consisted of a nurse, a physiotherapist, a biomedical professional, social workers, Social Work interns, a doctor, and a social director, per previously defined inclusion criteria:
1) Be a professional in health/education/assistance; 2) Be available to participate in program sessions and evaluations; 3) Have access to the internet, computer/cell phone/tablet, or any device that allows access to the program sessions online. The mean age of the participants was 43.6 years (SD= 15.86), with a minimum of 20 and a maximum of 62 years. The mean total working time in the functional/working life was 15.4 years (SD = 13.5) with a variation of 01-34 years of service, with a mean of 2.48 years in the current position (SD = 2.73). Six participants were married or in a common-law marriage, four had children, and two lived alone. Three participants were retired (due to age, contribution time, and particular case), and one was preparing for retirement. Three participants were caregivers of people they were close to. Nine participants reported experiencing some significant/impacting life event in the last year, and nine identified at least one source (person/institution) as a support network. Six participants had some type of belief or religion; five reported having chronic physical or mental health problems (anxiety with and without panic attacks, depression, stomach pain, cancer). Three participants reported that they were currently grieving a personal loss. All participants had some type of leisure activity, including reading/studying (4), engaging in physical activities (4) (walking (1), Pilates (1), gym (1), running (1)), watching movies/series (3), staying with family (2), traveling (2), dancing (1), volunteer work (1), watching decorating programs (1) listening to music (1), going to the movies (1), going out with friends (1), walking outdoors (1), eating (1).
Tools
We employed the following tools:
Sociodemographic data questionnaire (T1): Containing questions about age, sex, work aspects, schooling level, and family composition.
Program Evaluation Sheet (T2): Containing 12 objective self-reporting questions with answers ranging from 1-dissatisfied to 4-very satisfied, consisting of 6 questions that assess satisfaction with the program, the moderator, the schedule, the duration of the sessions, and the lessons learned from the program; 2 questions about clarity and understanding of the contents covered and 4 questions about generalization (application in life) of the contents covered in the program. Moreover, the instrument includes two descriptive questions asking for examples of program content used and suggestions/feedback for program improvements (Durgante et al., 2019b).
Moderator’s field diary: Used for records during and at the end of the sessions, based on the CRIF protocol’s criteria (Damschroder et al., 2009) for methodological quality in evaluating the program implementation process.
Procedures
The Ethics Committee of the Federal University of Rio Grande do Sul-UFRGS approved the research under Opinion N° 4.143.219. Initially, we contacted the management team of the retirees’ association to publicize the program. We adopted a bottom-up perspective based on direct involvement and collaboration with stakeholders at all stages of the research. Three meetings were held (2.30-3 h each) with the management team (N = 5) to make the proposal feasible with the association’s professionals. The different phases of the procedures (phase I, II, III, and IV), which include the preparation of the program and its implementation, results, and data discussion (phase V), are described below.
Phase I: Knowledge generation and collaboration with stakeholders
Based on the Intervention characteristics axis of the CFIR protocol, some questions were debated regarding the following criteria: evidence on the strength and quality of the intervention, with data on studies conducted, results obtained, and presentation of the program implementation manual; discussion about the advantages of implementing the intervention versus any alternative solution (Relative advantage) and about the potential adaptability of the intervention, the proposed activities, dynamics, schedules, approach to the themes for a differentiated target audience (professionals) of the original version of the program (older adults/retired); discussion about the possibility of conducting a study for a small group -directive and health management team- in a controlled environment, including the participants’ perception in the adaptation and implementation of the intervention (Trialability); discussion about the potential of the intervention to impair the institution’s routine work practices and actions necessary for the health management team to participate in the program (Complexity). This criterion relaxed access and in a joint decision with the health management team, the management team opted to allocate work hours/shifts so that professionals could participate in the program without compromising their work tasks. The participants themselves chose the shift and time for implementing the program. As for the Design quality and packaging criterion, we prepared a structured program project containing an introduction on health promotion issues and relevant literature, structure, method, and results. We presented the program manual and briefly discussed with the management team how the program could be implemented with the association.
Phase II: Integrating the information generated with theory and empirical and clinical knowledge
In this phase, Outer setting criteria were discussed with the management team, containing questions about the need for psychological support for the team in the face of growing health demands from the associates and the team, given the pandemic and possible topics to be addressed in the program, relevant to professionals and grounded on scientific literature, such as physical and mental exhaustion, irritability, sleep dysfunction/anxiety, service overload/long working hours, perception of impotence given the current health situation (patient needs and resources).
Regarding the Inner setting, the meetings addressed team issues about how much the intervention was as per the organizational culture (Culture) and Implementation climate since the program could be helpful, supported, and recognized as an input to the mental health of professionals (compatibility) who did not have a structured proposal to promote their health. The need to understand the receptivity and prioritization (relative priority) of the target audience after the program was announced was emphasized to have an idea about the demand for this type of service in this specific context. It is worth mentioning that the management team supported and encouraged the participation of professionals (organization incentives and rewards), which favored the subsequent implementation of the program.
After the initial meetings with the management team, the Characteristics of Individuals axis was perceived with greater knowledge to disseminate the program to the health management team (Knowledge and beliefs about the intervention).
Phase III: Reviewing and initiating the intervention in the adapted format with the stakeholders/target audience
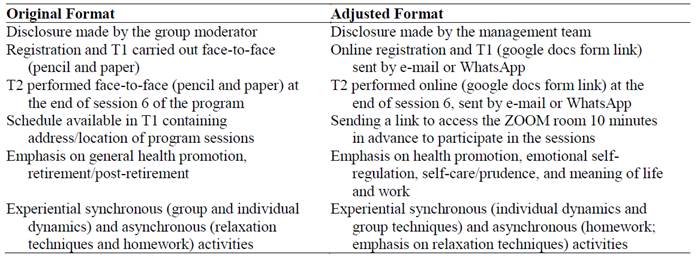
From the axes and criteria evaluated in the initial phases, based on the perception of the management team, we could introduce initial adaptations in the process (Axis: Process, criterion: planning) of selecting participants and topics of interest to the target audience, due to the historical moment of program implementation, when Brazil was one of the world epicenters of the COVID-19 pandemic. The adaptations include systematizing the activities before and during the program for online implementation and reviews and emphasis on topics of interest reported by the health management team. Table 1 presents the changes initially included for the online implementation of the program.
Phase IV: Conducting preliminary tests with the adapted version of the intervention
After the initial adjustments in the program’s structure, we conducted a group with the adapted version of the Vem Ser Program with the management team to evaluate the functionality of the adapted components of the program and some feasibility criteria as a preliminary assessment of this type of intervention. The online sessions were implemented on six consecutive Wednesdays, starting at 10 am. The mean duration of the sessions was 2.17 h (SD = 0.11). Session 5 (Theme: Forgiveness) was the shortest, lasting 2.08 h, and Session 6 (Theme: Meaning of Life and Work) was the most protracted, lasting 2.37 h , including the assessment of T2. Only one absence was recorded (Session 3: Empathy), which represents 98.3 % of attendance in the group. All participants (N = 10) completed the program and T2.
The outcome indicators evaluated followed the SMART criteria (specific, measurable, attainable, relevant, timely), proposed in the Process axis (reflecting and evaluating) (Damschroder et al., 2009). The demand was satisfactory since we observed a unanimous perception of the need for this type of intervention at this historical moment and specific context by the directive team and the health management team. All team professionals participated in the program voluntarily. A waiting list was prepared for other interested professionals, and the management team manifested interest and requested to offer the program to the association’s members (retired) in the future.
Phase V: Finalizing the culturally adapted version of the intervention
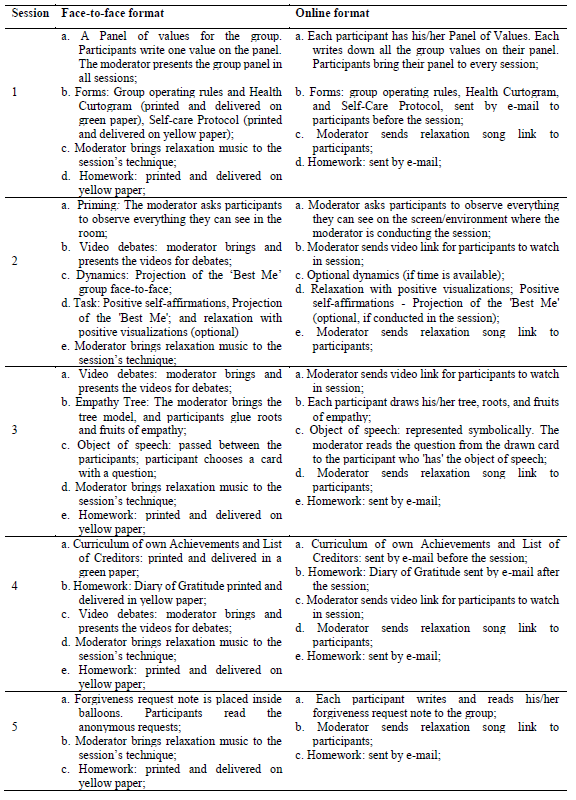
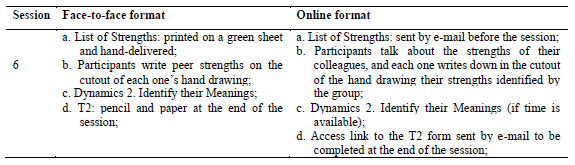
Changes were introduced in the structure, dynamics, and materials used in the sessions based on the process evaluation, per the moderator’s field diary, to enable online implementation, as illustrated in Table 2a T2b.
Results and Discussion
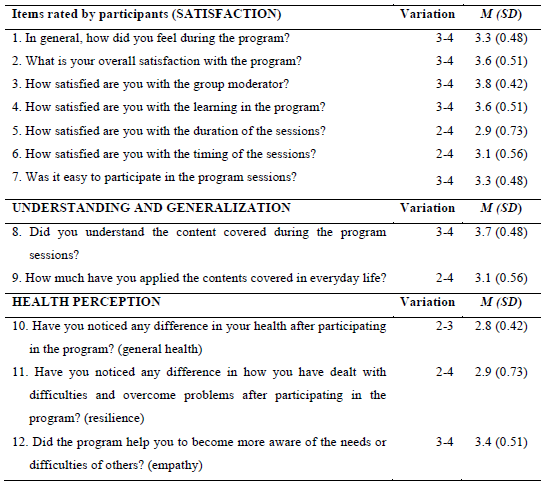
Table 3 shows variations in scores (between 1 and 4), means (M), and standard deviation (SD) of the objective questions of the participants’ evaluations regarding satisfaction with the program and the moderator, understanding, and generalization of the contents covered in the program and health issues, per the participants’ self-report.
The overall mean of participants’ satisfaction with the program was 3.37 (SD = 0.38), items from 1-7, with results ranging from 2 to 4 on a scale of 1 to 4 points, as in the comments: “The Distance Learning (DL) version of the program version was excellent. It worked perfectly, and I believe that can be put into practice immediately” (participant, 59 years old). “A wonderful experience that made me reflect on practical everyday things” (participant, 36 years old). “I really enjoyed the program. I think it was a vibrant space for debate, in which could see the other in a more “humane” way and address issues that we often avoid thinking about, but that are still necessary for our maturation and personal growth” (participant, 22 years old). “It was great to participate because I noticed the improvement in the sessions at all times. I could go back to moments still hurting me and understand the need to seek treatment. I started therapy last week, along with the sessions. It is making me almost become someone else: lighter, and less sad, worried and anxious” (participant, 20 years old).
The best-evaluated item relates to the participant’s satisfaction with the group moderator (M = 3.8; SD = 0.42). The least well-rated item was the participant’s satisfaction with the duration of the sessions (M = 2.9; SD = 0.73), “as a suggestion, I believe that smaller group sessions would streamline time and be even more productive” (participant, 36 years old). These results follow a pattern already identified in a feasibility study in the face-to-face version of the program (Durgante et al., 2019b). However, given the literature on the duration of interventions along these lines (Bolier et al., 2013; Durgante, 2017; Durgante et al., 2019a), in a group psychoeducational approach, with Cognitive-Behavioral Therapy (Neufeld & Rangé, 2017) approach, a maximum duration of 2 hours is suggested, and the moderator could divide the activities of the sessions into two (two meetings with the same theme). Alternatively, it is possible to reduce the number of participants in the groups so that all can present and share their experiences, as suggested by one participant... “sessions with a longer duration or smaller group to allow more space for speech” (participant, 32 years old).
The content generalization mean was 3.4 (SD = 0.39), ranging from 2 to 4. The contents used in life, as reported by the participants are: gratitude, “I used the gratitude diary a lot. I do it daily, and I already feel improvements concerning my anxiety” (participant, 22 years old); “I started to look more at my day to day, observing and thanking for all the little things” (participant, 59 years old). Empathy, “In the relationships with my daughter” (participant, 38 years old); “I started to observe the other’s perspective more” (participant, 59 years old); “A time when I fought with a close person and when I was a difficult person to live with at home. With empathy, I could understand people’s reasons for being sad. Thinking about the conflicts I had with them made me understand that my behavior was causing that, and being bad, I was putting a load on people and demanding perfection. It was excellent because the relationship with them totally changed” (participant, 20 years old). Forgiveness and self-forgiveness, “I reflected on things about my past that I needed to share with myself in forgiving myself in order to achieve closure” (participant, 59 years old); “Self-forgiveness, understanding my limitations and that I don’t need to please everyone” (participant, 32 years old). We also had suggestions about increasing the duration of the sessions or reducing the number of participants. People suggested including more group dynamics, “I loved the program; I would like it to be used for more dynamic group reflection” (participant, 57 years old).
Barriers and facilitators identified in the implementation process
As barriers identified in the implementation process, in the Characteristics of individuals axis, we could identify a dispute for ‘space’ and recognition of specific knowledge by a participant, which hindered the progress of some activities in the sessions, as in Session 2 (theme: Optimism). In this case, there was contestation and non-acceptance of the operational definition of the forces worked on in each session based on the empirical literature in the area, criticized Session 1 icebreaking sentence (theme: values and self-care), and some interventions underestimated the importance of contents and dynamics addressed in the sessions, which prolonged debates on concepts and the theoretical model used, which delayed the conclusion of the sessions. We could detect a discrepancy and paradigmatic clash between the biomedical-curative-hospital-centered model of health production and the health promotion model adopted in the Vem Ser Program, based on the Positive Psychology and Public Health-Collective Health prism (Campos, 2000), which may have triggered tension and resistance by this participant in his questions and reflections (other personal attributes). There was also resistance by this same participant to respect the delay tolerance time at the onset of the sessions, a criterion established by the group members collaboratively in Session 1 as a norm for the proper functioning of group work (Neufeld & Rangé, 2017). This impasse was mitigated from Session 3 onwards when the participant was not allowed to enter the session after exceeding the delay tolerance time for the third consecutive time.
On the other hand, regarding the Inner Context axis of implementation (Inner setting), regarding the Networks and communications criterion, we could observe group fluidity and cohesion for the dissemination of information through networks (WhatsApp groups and institutional e-mail), which facilitated the organization and implementation process, since links to access videos and materials were sent during the session and simultaneously redirected by colleagues to other participants who were using cell phones to access the sessions. Having a reference professional as a point of contact for the dissemination and a professional who helped with contacts with the health management team members during the sessions accelerated the speed of communication and information transfer. In this sense, research indicates that the relationship established between members in institutions regarding collaboration and cooperation becomes more important than individual attributes (Wierenga et al., 2013), which helps with a sense of team/community and facilitates the process of implementing health interventions in these settings. Thus, strengthening collective sense and group cohesion can facilitate health promotion interventions in organizational and work contexts.
Regarding costs, axis: Intervention characteristics; criterion: Cost (base year: 2020), we should remember that this was the first online intervention proposal with the program after the onset of the pandemic and, for this reason, we had emergency investments for the acquisition of materials. We had a financial investment to cover the monthly fee for the online platform and materials for use in the sessions. However, these will serve for future research with the program and subsequent online implementation in different groups. Therefore, the costs associated with the implementation can be interpreted as investments that will support the continuity of research and assistance to the population in general. Given the problematic pandemic situation, we hope these experiences can help streamline research and health work investments.
Final considerations
This is the first national study based on two internationally recognized protocols for adapting interventions to different settings and populations. Using guide protocols for adapting interventions to other contexts and cultures is a fundamental practice. However, it has been barely observed in implementation research (Damschroder et al., 2009; Hwang, 2009). Many interventions with innovative potential, which could serve as robust resources for health, fail in their clinical usefulness, mainly due to low methodological quality and lack of use of scientifically based criteria and strategies for adapting interventions to other contexts and populations.
We should remember that there are different protocols for adapting interventions, and the researcher should identify the most suitable for their proposal, context, culture, historical-social moment, and target population whose intervention is targeted (Stoner et al., 2020). The cost analysis enabled us to suggest possibilities for streamlining resources associated with the implementation. As it is an online intervention, costs with the travel of the team and the participants, acquisition of printed materials such as evaluation protocol, session sheets, and homework were non-existent, which configures this intervention modality of the Vem Ser Program as low-cost. This criterion is poorly evaluated and reported, since it is associated with efficiency, and evaluations often focus on intervention efficacy and effectiveness criteria.
As limitations of this study, we emphasize that it was impossible to evaluate some CFIR criteria, such as Cosmopolitanism, Peer pressure, External policies, and incentives, from the Outer Setting axis; Individual identification with the organization, Individual stage of change, Self-efficacy, from the Characteristics of Individuals axis. These data remain to be investigated in future feasibility studies of the intervention in its online version. We also have the specific context in which the intervention was adapted, as it is an association of retired employees, which inhibits the possibility of generalizing the results obtained to other contexts. This direct us to follow up the research with the intervention in the online format, including different samples, control group, and different group moderators, and the verification of efficacy criteria for health promotion more broadly.
However, through the rigor and systematization used in the process of adapting the Vem Ser Program to the online version described in this paper, this effort is expected to favor new interventional work in a national context, given the scientificity required for adaptations and adjustments of interventions and that it is more likely to be effective in different contexts and for different populations.
REFERENCES
Bolier, L., Haverman, M., Westerhof, G. J., Riper, H., Smit, F., & Bohlmeijer, E. (2013). Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health, 13, 119. doi.org/10.1186/1471-2458-13-119 [ Links ]
Campos, G. W. de S. (2000). Saúde pública e saúde coletiva: campo e núcleo de saberes e práticas. Ciência & Saúde Coletiva, 5(2), 219-230. https://doi.org/10.1590/s1413-81232000000200002 [ Links ]
Cohn, M. A., & Fredrickson, B. L. (2010). In search of durable positive psychology interventions: Predictors and consequences of long-term positive behavior change. Journal of Positive Psychology, 5(5), 355-366. https://doi.org/10.1080/17439760.2010.508883 [ Links ]
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science, 4(1), 50. https://doi.org/10.1186/1748-5908-4-50 [ Links ]
Driggin, E., Madhavan, M. V., Bikdeli, B., Chuich, T., Laracy, J., Bondi-Zoccai, G., Brown, T. S., Der Nigoghossian, C., Zidar, D. A., Haythe, J., Brodie, D., Beckman, J. A., Kirtane, A. J., Stone, G. W., Krumholz, H. M., & Parikh, S. A. (2020). Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems during the Coronavirus Disease 2019 (COVID-19) Pandemic. Journal of the American College of Cardiology, 2019. https://doi.org/10.1016/j.jacc.2020.03.031 [ Links ]
Duan, Y., Zhu, H.-L., & Zhou, C. (2020). Advance of promising targets and agents against 2019-nCoV in China. Drug Discovery Today, 00(00), 10-12. https://doi.org/10.1016/j.drudis.2020.02.011 [ Links ]
Durgante, H. B. (2017). Qualidade metodológica de programas de intervenção baseados em fortalezas na América Latina: uma revisão sistemática da literatura. Contextos Clínicos, 10(1), 2-22. https://doi.org/10.4013/ctc.2017.101.01 [ Links ]
Durgante, H. & Dell’Aglio, D. D. (2019). Multicomponent positive psychology intervention for health promotion of Brazilian retirees: a quasi-experimental study. Psicologia: Reflexão e Critica, 32(1). https://doi.org/10.1186/s41155-019-0119-2 [ Links ]
Durgante, H., Mezejewski, L. W., Sá, C. N., & Dell’Aglio, D. D. (2019a). Intervenciones psicológicas positivas para adultos mayores en Brasil. Ciencias Psicológicas, 13(1), 106-118. https://doi.org/10.22235/cp.v13i1.1813 [ Links ]
Durgante, H., Naveire, C., & Dell’Aglio, D. (2019b). Psicologia positiva para promoção de saúde em aposentados: estudo de viabilidade. Avances En Psicología Latinoamericana, 37(2), 269-281. https://doi.org/10.12804/revistas.urosario.edu.co/apl/a.6375 [ Links ]
Durgante, H., Mezejewski, L.W., & Dell’Aglio, D.D. (2020a). Desenvolvimento de um Programa de Psicologia Positiva para promoção de saúde de aposentados. Programa Vem Ser. Em C. H. Giacomoni & F. Scorsolini-Comin (Eds.), Temas especiais em Psicologia Positiva (pp. 188-202). Editora Vozes. [ Links ]
Durgante, H. B., Tomasi, L. M. B., Pedroso de Lima, M. M., & Dell’Aglio, D. D. (2020b). Long-term effects and impact of a positive psychology intervention for Brazilian retirees. Current Psychology, 41, 1504-1515. https://doi.org/10.1007/s12144-020-00683-7 [ Links ]
Ebert, D. D., Cuijpers, P., Muñoz, R. F., & Baumeister, H. (2017). Prevention of mental health disorders using internet- and mobile-based interventions: A narrative review and recommendations for future research. Frontiers in Psychiatry, 8(AUG). https://doi.org/10.3389/fpsyt.2017.00116 [ Links ]
Firth, J., Torous, J., Nicholas, J., Carney, R., Pratap, A., Rosenbaum, S., & Sarris, J. (2017). The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry, 16(3), 287-298. https://doi.org/10.1002/wps.20472 [ Links ]
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., Zhang, L., Fan, G., Xu, J., Gu, X., Cheng, Z., Yu, T., Xia, J., Wei, Y., Wu, W., Xie, X., Yin, W., Li, H., Liu, M., Xiao, Y., … Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 395(10223), 497-506. https://doi.org/10.1016/S0140-6736(20)30183-5 [ Links ]
Hwang, W. C. (2009). The Formative Method for Adapting Psychotherapy (FMAP): A community-based developmental approach to culturally adapting therapy. Prof Professional Psychology Research and Practice, 40(4), 369-377. https://pubmed.ncbi.nlm.nih.gov/20625458/ [ Links ]
Knapp, P. & Beck, A. T. (2008). Cognitive therapy: foundations, conceptual models,applications and research. Revista Brasileira de Psiquiatria, 30(Suppl II), 54-64. [ Links ]
Magyar-Moe, J. L., Owens, R. L., & Conoley, C. W. (2015). Positive Psychological Interventions in Counseling: What Every Counseling Psychologist Should Know. The Counseling Psychologist, 43(4). [ Links ]
Marasca, A. R., Yates, D. B., Schneider, A. M. de A., Feijó, L. P., & Bandeira, D. R. (2020). Avaliação Psicológica On-line: considerações a partir da pandemia do novo coronavírus (Covid-19) para a prática e o ensino no contexto à distância. Revista Estudos Em Psicologia (Campinas), Pré-print, 1-24. https://doi.org/10.1590/SciELOPreprints.492 [ Links ]
Mouton, A. & Cloes, M. (2013). Web-based interventions to promote physical activity by older adults: promising perspectives for a public health challenge. Arch Public Health, 71(16). https://doi.org/10.1186/0778-7367-71-16 [ Links ]
Neufeld, C. B. & Rangé, B. P. (2017). Terapia cognitivo-comportamental em grupos: das evidências à prática. Artmed. [ Links ]
Nikrahan, G. R., Suarez, L., Asgari, K., Beach, S. R., Celano, C. M., Kalantari, M., Abedi, M. R., Etesampour, A., Abbas, R., & Huffman, J. C. (2016). Positive Psychology interventions for patients with heart disease: a preliminary randomized trial. Psychosomatics, 57(4), 348-358. https://doi.org/10.1016/j.psym.2016.03.003 [ Links ]
Northouse, L., Schafenacker, A., Barr, K. L. C., Katapodi, M., Yoon, H., Brittain, K., Song, L., Ronis, D. L., An, L. (2014). A Tailored Web-Based Psychoeducational Intervention for Cancer Patients and Their Family Caregivers. Cancer Nursing, 37(5), 321-330. https://doi.org/10.1097/ncc.0000000000000159 [ Links ]
Proyer, R. T., Gander, F., Wellenzohn, S., & Ruch, W. (2014). Positive psychology interventions in people aged 50-79 years: long-term effects of placebo-controlled online interventions on well-being and depression. Aging and Mental Health, 18(8), 997-1005. https://doi.org/10.1080/13607863.2014.899978 [ Links ]
Reppold, C. T., Gurgel, L. G., & Schiavon, C. C. (2015). Research in positive psychology: a systematic literature review. Psico USF, 20(2), 275-285. [ Links ]
Richard, E., Moll van Charante, E. P., Hoevenaar-Blom, M. P., Coley, N., Barbera, M., Van der Groep, A., Meiller, Y., Mangialasche, F., Beishuizen, C. B., Jongstra, S., Van Middelaar, T., Van Wanrooij, L. L., Ngandu, T., Guillemont, J., Andrieu, S., Brayne, C., Kivipelto, M., Soininen, H., Van Gool, W. A. (2019). Healthy ageing through internet counselling in the elderly (HATICE): a multinational, randomised controlled trial. The Lancet Digital Health, 1(8), e424-e434. https://doi.org/10.1016/S2589-7500(19)30153-0 [ Links ]
Rogers, M. A. M., Lemmen, K., Kramer, R., Mann, J., & Chopra, V. (2017). Internet-delivered health interventions that work: Systematic review of meta-analyses and evaluation of website availability. Journal of Medical Internet Research, 19(3), 1-28. https://doi.org/10.2196/jmir.7111 [ Links ]
Saldaña, J. (2009). The coding manual for qualitative researchers. Sage [ Links ]
Sin, N. L. & Lyubomirsky, S. (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467-487. https://doi.org/10.1002/jclp.20593 [ Links ]
Spina, S., Marrazzo, F., Migliari, M., Stucchi, R., Sforza, A., & Fumagalli, R. (2020). The response of Milan’s Emergency Medical System to the COVID-19 outbreak in Italy. The Lancet, 395(10227), e49-e50. https://doi.org/10.1016/S0140-6736(20)30493-1 [ Links ]
Stoner, C. R., Chandra, M., Bertrand, E., Du, B., Durgante, H., Klaptocz, J., Krishna, M., Lakshminarayanan, M,, Mkenda, S., Mograbi, D. C., Orrell, M., Paddick, S-M., Vaitheswaran, S., Spector, A. (2020). A New Approach for Developing “Implementation Plans” for Cognitive Stimulation Therapy (CST) in Low and Middle-Income Countries: Results From the CST-International Study. Frontiers in Public Health, 8(July), 1-11. https://doi.org/10.3389/fpubh.2020.00342 [ Links ]
Watkins, J. (2020). Preventing a covid-19 pandemic. The BMJ, 368. https://doi.org/10.1136/bmj.m810 [ Links ]
Welch, V., Petkovic, J., Pardo Pardo, J., Rader, T., & Tugwell, P. (2016). Interactive social media interventions to promote health equity: An overview of reviews. Health Promotion and Chronic Disease Prevention in Canada, 36(4), 63-75. https://doi.org/10.24095/hpcdp.36.4.01 [ Links ]
Wierenga, D., Engbers, L. H., Van Empelen, P., Duijts, S., Hildebrandt, V. H., & Van Mechelen, W. (2013). What is actually measured in process evaluations for worksite health promotion programs: A systematic review. BMC Public Health , 13(1). https://doi.org/10.1186/1471-2458-13-1190 [ Links ]
World Health Organization. (2020a). Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-26-march-2021 [ Links ]
World Health Organization. (2020b). Mental health and psychosocial considerations during COVID-19 outbreak. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf [ Links ]
How to cite: Durgante, H. B. & Dell’Aglio, D. D. (2022). Adaptation for online implementation of a Positive Psychology intervention for health promotion. Ciencias Psicológicas, 16(2), e-2250. https://doi.org/10.22235/cp.v16i2.2250
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. H. B. D. has contributed in a, b, c, d, e; D. D. DA. in a, c, e.
Received: August 27, 2020; Accepted: June 14, 2022











 texto en
texto en