Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Ciencias Psicológicas
versión impresa ISSN 1688-4094versión On-line ISSN 1688-4221
Cienc. Psicol. vol.13 no.2 Montevideo dic. 2019 Epub 01-Dic-2019
https://doi.org/10.22235/cp.v13i2.1894
Original Articles
Post-traumatic stress disorder in abused Spanish children
1Facultad de Psicología. Universidad de Murcia. España
2 Asociación para el Desarrollo de la Salud Mental en Infancia y Juventud, “Quiero Crecer”, Murcia. España, maracastro@um.es, amperez@um.es, clopezs@um.es, jjlopga@um.es, mavialcantara@um.es
Keywords: child abuse; intimate partner violence exposure; children in care; PTSD; DSM
Palabras clave: abuso infantil; exposición a violencia de género; menores tutelados; TEPT. DSM
Introduction
Numerous prospective and retrospective studies have found that one of the most common consequences associated with child abuse is Post-Traumatic Stress Disorder (PTSD) (e.g., Shenk, Putnam, & Noll, 2012; Tolin & Foa, 2006).
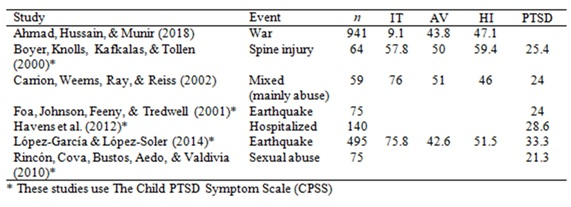
The percentages of children with PTSD in the general population are variable, finding a range from 1.6% to over 6% (Essau, Conradt, & Peterman, 2000; Furtado, Carvalhães, & Gonçalves, 2009). In a clinical population, the prevalence of PTSD symptoms is higher among individuals who have been exposed to a traumatic life event (see Table 1). Alisic et al. (2014) carried out a meta-analytic study and found that 15.9% of children exposed to trauma presented PTSD following DSM-IV criteria (APA, 1991). However, when using the DSM criteria, rates and prevalence of PTSD are very low, which may be a result of the strict criteria which is specifically designed for adults (Scheeringa, Wright, Hunt, & Zeanah, 2006).
In addition to the classic categories of maltreatment (physical, sexual, and emotional abuse and neglect), exposure to intimate partner violence (IPV) against women is also considered to be a form of child abuse (WHO, 2016). It has been widely documented throughout the scientific literature that children exposed to IPV are more likely to present problems in multiple areas of development (Castro et al., 2017; Howell, Barnes, Miller, & Graham-Bermann, 2016). What is not clear is the severity of this type of abuse compared to direct abuse suffered at home, specifically among children living with their mothers who have been victims of IPV, and whether or not a mother in this situation would still be able to protect her child from developing mental health disorders.
Research has supported the claim that abused children who are living outside of the family home and who are made wards of the state present more clinically severe mental health problems than do those who remain with their family of origin (Burns et al., 2004). For example, Kolko et al. (2009) found that children in care (CIC) show a higher PTSD symptomatology than those who continue living with their biological parents. Their sample consisted of 1,848 Americans between the ages of 8 and 14 divided into two groups: 483 CIC participants (group I) and 1,365 participants who were beneficiaries of the Child Protective Services, but who remained with their biological parents (group II). Participants varied in the specific forms of abuse that they had each endured. Results from this study showed statistically significant differences between the two groups, both in their average scores and prevalence rates of PTSD. Oswald et al. (2010) found similar results in their study comparing two groups of Germans between the ages of 7 and 16: a control group comprised of participants who had lived with at least one of their biological parents, and another group which included CIC. Their results showed that the group of CIC had a significantly higher prevalence of PTSD symptoms than did the children in the control group.
These results may be partially explained by the role of the non-abusive parent as a resilience factor to help prevent the child from developing PTSD. Numerous studies suggest that having at least one stable and long-lasting, meaningful relationship with an adult can provide a child with the comfort and positive reinforcement needed to buffer against harmful outcomes which may otherwise result from continuous exposure to abuse (Aguilar, 2001). This type of positive relationship is commonly formed between a child and one of his or her parents (Osofsky, 2003). Research has shown that a child with a caregiver who attends to and meets his or her needs is less likely to develop psychological problems than are children without this form of support (Øverlien, 2010).
Research suggests that a mother’s parental role, even among those who are victims of IPV, may protect the child from developing more psychological problems (Fong, Hawes, & Allen, 2017; Manning, Davies, & Cicchetti, 2014). However, the protective role of the mother is frequently hindered by the deleterious effects that IPV has on women in terms of their emotional and physical wellbeing (Boeckel, Wagner, & Grassi-Oliveira, 2017). What is less known is whether or not these negative outcomes are significant enough to completely block a mother’s ability to serve as a resilience factor.
In many cases, CIC are deprived of the opportunity to receive any protection or support from an adult family member. Numerous researchers, such as Legault, Anawati and Flynn (2006), have highlighted the role of the educator as a potential resilience factor for a child. However, studies have indicated that it may be difficult for educators to fully assume this role due to the high level of distress and emotional exhaustion associated with mentoring and supporting children in this given situation (Gibbs, 2001). Therefore, these supportive relationships may be partially or entirely inaccessible to CIC, which may result in fewer protective factors to buffer against the development of psychological problems among CIC. Although there are numerous studies on PTSD in abused children, in Spain there are no systematic studies using DSM criteria and validated and reliable instruments to provide specific data on this issue.
The present study aims to investigate the prevalence of Post-Traumatic Stress Disorder, in Spanish children who have suffered chronic abuse, and to establish differences in the symptomatology and complete diagnosis of PTSD between CIC who have suffered various forms of chronic abuse and children who have been exposed to IPV. Based on the scientific literature, we hypothesized that CIC would show higher rates of PTSD than would children exposed to IPV who were living with their biological families, and both present much higher prevalence in the general population.
Materials and method
Participants
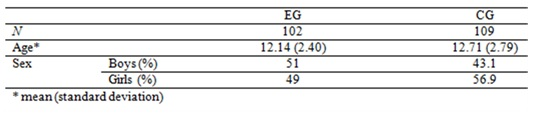
The sample consisted of a total of 211 children between the ages of 8 and 17. The control group (CG) consists of 109 children and the abuse group (EG) consists of 102 children (see Table 2).
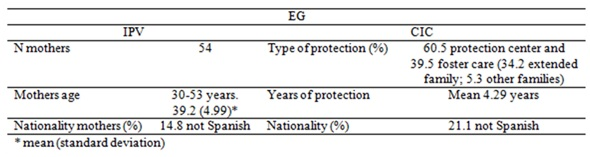
The children of the exposed group had been exposed to domestic violence and presented signs of serious psychological alterations at the time of the initial evaluation. The group of abused children was divided in two subgroups. Subgroup IPV consisted of 64 children who received indirect abuse because they have been exposed to intimate partner violence (IPV) against their mothers. These children were living at the time with their biological family, specifically their mother in many cases, and had been assigned to the Psychological Intervention for Child Intimate Violence Victims Service (SAPMEX). Subgroup CIC consisted of 38 children in care (CIC) from the Region of Murcia due to their parents having lost custody of their children, who were assigned to the Project of Evaluation, Diagnosis and Psychological Intervention for CIC (PEDIMET) (see Table 3).
The selection of the control group, with ages between 8 and 17 years old, was organized in state schools and secondary schools in the Region of Murcia, and 20% were not of Spanish nationality.
Instrument
The Child PTSD Symptom Scale (CPSS) (Foa et al., 2001) is a specific instrument used to evaluate the presence of PTSD symptoms in children and teenagers aged 8 to 18 years. The measure can be used as a form of self-report or as a structured clinical interview (Foa et al., 2001) and is based on the PTSD diagnostic criteria of the DSM-IV-TR (APA, 2000). Currently, the scale is being adapted to DSM-5 criteria (APA, 2013), however, the Spanish version is not available yet (Foa, Asnaani, Zang, Capaldi, & Yeh, 2018).
The CPSS is a 24-item-questionnaire regarding a specific traumatic event experienced. The measure is divided into two parts: part I consist of 17 items evaluating event-consequential symptoms, and part II consists of 7 items evaluating the degree of interference of the symptomatology in different areas of life. The response format is in a 4-point Likert-type scale ranging from 0 to 3 (where 0=Not at all/only once; 1=Once a week/once in a while, 2=Two to four times a week/half of the time; 3=Five or more times a week/almost always). The measure consists of three subscales based on criteria clusters (Intrusive Thoughts in 5 items; Avoidance in 7 items; Hyperarousal with 5 items) that can be scored dichotomously (Yes/No) as they reach PTSD diagnosis criteria (Foa et al., 2001).
The psychometric properties of the CPSS indicate appropriate levels of reliability (Bustos, Rincón, & Aedo, 2009; Foa et al. 2001; Havens et al., 2012; Serrano-Ibañez, Ruiz-Párraga, Esteve, Ramírez-Maestre, & López-Martínez, 2018; Venta, & Mercado, 2019).
In this study, the level of reliability of the CPSS for the total of the first part of the scale was high in both the abuse group (.89) (N=102) and control group (.78) (N=109). The subscales’ levels of reliability were as follows: Intrusive Thoughts (.81EG; .63 CG), Avoidance (.73 EG; .50 CG) and Hyperarousal (.77 EG; .61 CG).
Procedure
In the EG, participants in EG1 consisted of children recruited through the SAPMEX Service at the Spanish Association for the Development of Mental Health in Childhood and Youth, “I Want to Grow”, by psychologists who worked with the children´s mothers in the Centers for Domestic Violence. The children participating in these studies were recruited from the 169 cases referred to the Service between July 2009 and October 2010. Of these, 105 were excluded because they did not meet the criteria for the study.
Participants in EG2 consisted of children recruited from the PEDIMET Program for Children in Care of the University of Murcia, by Child Protection Service psychologists The children participating in these studies were recruited from the 117 cases referred to the Program between January 2005 and October 2008. Of these, 79 were excluded because they did not meet the criteria for the study.
We received detailed reports of the children, which were either compiled by the psychologists who worked with the mothers (EG1), or by the Child Protection Service psychologist (EG2). These reports included the most pertinent information about the child as well as his or her history of exposure to different types of abuse. While following a protocol designed for working with abused children, initial psychological evaluations were administered to the participants. After the initial evaluation, we applied specific psychological tests which corresponded to the psychological problems that were observed and evaluated by psychologist in each child. Assessment of PTSD by CPSS was conducted as interview each child individually.
The following inclusion criteria were established and applied at the time of the initial evaluation: A) the child’s mother was a victim of IPV, the child was being exposed to the violence, and either the mother was being taken care of in the Centers for Domestic Violence (group I) or the child was a CIC of the Region of Murcia) (group II); B) the child had internalizing and/or externalizing symptoms moderate or severe gravity that interfere in his/her personal, family, social and/or school adjustment. C) the child was at least 8 years old. The established exclusion criteria were: the child presented developmental delays, Autism Spectrum Disorder (ASD), and/or psychosis. In all cases, informed consent and standards of confidentiality were implemented and thoroughly explained to the institution or child’s legal guardian.
Design and data analysis
This study follows an ex post facto design which was used to evaluate a sample of children who had been exposed to domestic abuse. The children were first assessed in order to evaluate their levels of psychological distress related to their histories of abuse. The children were then classified into two groups based upon the type of abuse that they had suffered. The study was designed to measure the prevalence of PTSD symptoms and their clinical diagnosis in order to assess differences between groups.
For the statistical analysis of the data, we used the 24th version of SPSS. The following procedures were applied:
Results
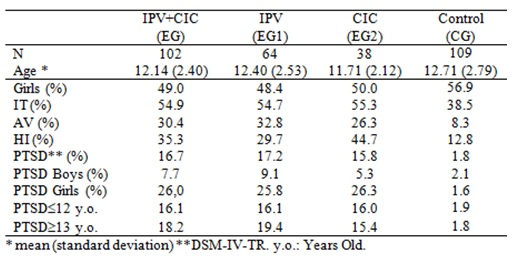
We calculated the prevalence of PTSD using the CPSS scale and subscales for the group of abused children (EG), IPV and CIC, and the control group (CG).
For the PTSD diagnosis, we followed the PTSD DSM-IV-TR Diagnostic Criteria (APA, 2000), which require persistent symptomatology of at least 1 symptom of Intrusive Thoughts (IT), 3 symptoms of Avoidance (AV), and 2 symptoms of Hyperarousal (HI). Based on these criteria, a symptom is considered to be present when it obtains a score of 2 or higher on the scale, indicating that the individual experiences the symptom at least 2 times per week.
Table 4 presents a summary of the results found. Regarding the diagnosis of PTSD, a prevalence rate of 16.7% was returned for the total number of abused children. When analyzing symptomatic groups, a greater prevalence of Intrusive Thoughts was observed (54.9%), followed by Hyperarousal (35.3%) and Avoidance (30.4%). In EG1, for children who had witnessed their mothers being victims of IPV, the prevalence of PTSD was 17.2%. When analyzing the prevalence of PTSD symptoms in each symptomatic group, we found that 54.7% experienced Intrusive Thoughts, 32.8% presented symptoms of Avoidance, and 29.7% showed significant signs of Hyperarousal. In EG2, the prevalence of a PTSD diagnosis among CIC was 15.8%. Regarding the groups of symptom scales, a greater prevalence of Intrusive Thoughts was noted (55.3%), followed by Hyperarousal (44.7%), and to a lesser extent Avoidance (26.3%). Moreover, in the control group found a prevalence of PTSD according to DSM 1.8%. When analyzing symptomatic groups, a greater prevalence of Intrusive Thoughts was observed (38.5%), followed by Hyperarousal (12.8%) and Avoidance (8.3%).
The PTSD in IPV prevalence is significantly higher than that observed in the control group/=13.676; p(.000; OR=11.104; IC95%: 2.375 - 51.908). However, the PTSD prevalence of IPV did not differ significantly from that found in CIC ( =0.034; p=.855). There is a significant effect due to sex, with a higher prevalence in girls than in boys, both IPV and CIC, but not in the control group. Considered separately, there were no differences in boys between the three groups, while in girls the percentage of PTSD in IPV was significantly different from the control group ( =13.839; p(.000; OR=21.217; IC95%: 2.513 - 178.160). Similarly, girls in the CIC, the prevalence of PTSD is higher than the control group ( =12.939; p(.000; OR=21.786; IC95%: 2.356- 201.435). Finally, there were no differences in girls between IPV and PTSD CIC.
Finally, to test the hypothesis of the study, we ran a Z-test test to check proportions of Intrusive Thoughts (IT), Avoidance (AV), Hyperarousal (HI), and total PTSD according to the DSM-IV-TR (1IT-3AV-2HI) between subgroup 1 (children exposed to IPV) and subgroup 2 (CIC). The results do not show statistically significant differences between the two groups, neither in the prevalence of the symptomatology in the subscales (IT, AV, and HI), nor in the diagnosis of PTSD. Therefore, we were unable to confirm the hypothesis.
Discussion
The study aimed to identify PTSD symptoms and diagnosis prevalence in children who have suffered chronic abuse, including exposure to IPV, as well as to assess any differences among the various forms of abuse experienced, either direct (as in the sample of CIC) or indirect (as in the sample of children exposed to IPV).
Regarding the groups of symptoms analyzed, 54.9% of the total sample of abused children (54.7% of children exposed to IPV; 55.3% of CIC) were found to have at least 1 symptom of Intrusive Thoughts. Boyer et al., (2000) found a similar percentage (57.8%) in patients with spinal injuries. Other studies found higher prevalence rates of individuals experiencing Intrusive Thoughts. For example, López-García & López-Soler (2014) studied a sample of people exposed to an earthquake and found that 75.8% reported Intrusive Thoughts. Carrion et al. (2002) used a different measure, and found that 76% of their clinical sample had experienced Intrusive Thoughts. Nevertheless, Ahmad et al. (2018) observed a lower prevalence rate (9.1%) comparing with our study. Regarding the 3 symptoms of Avoidance, we found a prevalence rate of 30.4% in the total sample (32.8% in children exposed to IPV; 26.3% in CIC), which is lower than those found in the four studies previously mentioned (Ahmad et al., 2018; Boyer et al., 2000; Carrion et al., 2002; López-García & López-Soler, 2014). Lastly, 35.3% of the total sample of children showed at least 2 symptoms of Hyperarousal. We observed a lower prevalence rate of Hyperarousal symptoms in the group exposed to IPV (29.7%) than in the group of CIC (44.7%). Again, the percentages of Hyperarousal found in our sample are lower than those found in other studies, which showed prevalence rates of 59.4% among patients with spinal injuries (Boyer et al., 2000), 46% in a clinical sample (Carrion et al., 2002), 47.1% in children displaced by conflict (Ahmad et al., 2018) and 51.5% in patients exposed to an earthquake (López-García & López-Soler, 2014). Overall, we found that our sample presented lower rates of PTSD symptoms than the participants with spinal injury (Boyer et al., 2000), those exposed to an earthquake (López-García & López-Soler, 2014), or a clinical sample (Carrion et al., 2002).
A comparison of the percentages found for each subgroup of PTSD symptoms is pertinent to highlight that both in our total sample and in the subsamples, the criterion cluster with the highest prevalence was Intrusive Thoughts. Carrion and colleagues (2002), who investigated a clinical sample, López-García & López-Soler (2014), who studied individuals who had experienced an earthquake, and Cedric & Goldbeck (2016) with traumatized children, found similar results in their studies. However, Boyer and colleagues (2000) and Ahmad et al. (2018) found that, in spinal injuries and minors displaced by conflict respectively, the most frequent symptomatology was Hyperarousal.
In this study, in subgroup 1 (children exposed to IPV), the second most frequent symptom was Avoidance and least frequent was Hyperarousal, which was also found by Carrion and colleagues (2002) and Ahmad and colleagues (2018). However, in subgroup 2 and in the total sample, the second highest prevalence was Hyperarousal, as in López-García & López-Soler (2014).
To summarize, we have highlighted the obtained profiles for each group. In subgroup 1, the order of criteria clusters based on prevalence rates was IT-AV-HI (ranging from higher to lower prevalence rates). This profile is comparable to the results gathered by Carrion and colleagues (2002) in a clinical sample. The profile obtained for children in subgroup 2 of our study was IT-HI-AV, which was similar to the results reported by López-García et al. (2012). Both profiles differ from those obtained by Boyer and colleagues (2000), which was HI-IT-AV, and by Ahmad et al. (2018), which was HI-AV-IT. These results may indicate the ineffectiveness of avoidance responses in situations where the source of stress is inevitable, as is the case of children exposed to direct abuse or those suffering from spinal injuries.
Following the PTSD DSM-IV-TR diagnostic criteria for PTSD (meeting criteria for all 3 groups of symptoms), our obtained prevalence was 17.2% for subgroup 1, 15.8% for subgroup 2, and 16.7% in total sample. These rates are higher than those found in the general population, which ranges from 1.6% to 6.3% (Essau et al., 2000; Furtado, Carvalhães, & Gonçalves, 2009). Our results are similar to Alisic et al. (2014) meta-analysis (15.9% average) and to those shown by using the same scale in other samples, for example among children with spinal injuries (Boyer et al., 2000), although their criterion differed in that it required at least 3 out of 4 symptoms (IT, AV, HI, and deterioration) to be present. Rincón et al., (2010) studied sexually abused children and found the prevalence of PTSD to be 21.3%. Other studies found higher percentages of PTSD in their samples. For example, in two separate studies which evaluated individuals who had experienced an earthquake, Foa and colleagues (2001) found 24% of their sample had PTSD, and López-García & López-Soler, 2014) found a prevalence of PTSD to be 33.3%. Havens and colleagues (2012) also found a higher prevalence of PTSD (28.6%) among their clinical sample.
In this study we hypothesized that CIC, which are typically children who do not live with and are not in contact with their biological family and who may undergo multiple types of abuse over longer periods of time, would show a greater prevalence of PTSD than would children exposed to IPV who live with their biological family. Only two studies with this specific research focus were found in the scientific literature (Kolko et al., 2009; Oswald et al., 2010). The results obtained did not confirm our hypothesis given that the differences in the symptomology and diagnosis of PTSD (using DSM-IV-TR criteria) were not significant between groups.
These results indicate that the symptomatology of PTSD remains at a similar level among these two groups of children. These findings are surprising given that the children in subgroup 1 who had been exposed to IPV were living with their biological mother (a potentially supportive attachment figure and resilience factor) and were more commonly the victims of indirect rather than direct victimization. This is in comparison to CIC in subgroup 2, which were children who did not live with biological family members and who, in many cases, had undergone various types of direct abuse. This is even more surprising when considering the fact that within subgroup 1, the mother and child were not living in a shelter home. Rather, in most cases, the mother and child were living with other family members, which could potentially provide even more support and protection for the child.
One possible explanation for this occurrence may be that in subgroup 1, even though the child’s mother is separated from the abuser, who in most cases was the father, she still may still undergo painful experiences (i.e., encounters with the abuser, changing her residence, dealing with the father being in prison, etc). Another possible explanation is that the mother may be unable to fulfill her role as a protective agent for her child due to the negative outcomes associated with being a victim of IPV.
It is important to emphasize the fact that the children who do not differ in PTSD symptomatology are not necessarily equal in terms of their clinical problems. One hypothesis would be that CIC show higher comorbidity and, regarding post-traumatic stress, they tend to present more complex trauma or developmental trauma than PTSD. What is confirmed here is that children exposed to IPV are victims of abuse. Undoubtedly, more investigations are required to give soundness and clarity to these findings and to answer the remaining questions, but children abused need efficacy treatment and stability in their lives.
Conclusions
Our study shows the importance of raising social support on serious posttraumatic reactions experienced by children exposed to violence against their mothers. Right decisions at the judicial level, especially in the regulation of custody, which result in greater protection and safety of children and minimize its consequences are required. Therefore, greater coordination between the judicial and social services in the issue of partner violence, as indicated Cala, Trigo, & Saavedra (2016), is necessary.
In conclusion, this study responds to a number of current needs in the field of child PTSD, making the following contributions: a) data on PTSD in Spanish children; b) prevalence data in children exposed to intimate partner violence; c) high involvement of children exposed to intimate partner violence in PTSD, no differences with children in care, indicating that those who have been exposed to intimate partner violence are also abused children; d) greater involvement of girls in PTSD symptoms
REFERENCES
Aguilar, L. (2001). La exposición a la violencia de género en el ámbito familiar: una forma de maltrato infantil. Recuperado de http://www.bienestaryproteccioninfantil.es/imagenes/tablaContenidos03SubSec/VG_casomaltrato.pdf [ Links ]
Ahmad, N., Hussain, S, & Munir, N. (2018). A tale of internal displacement: Post Traumatic Stress Disorder (PTSD) among school students in Swat, Pakistan. Rawal Medical Journal, 43 (3), 511-514. [ Links ]
Alisic, E., Zalta, A., Van Wesel, F., Larsen, S., Hafstad, G., Hassanpour, K., & Smid, G. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. British Journal of Psychiatry, 204 (5), 335-340. doi:10.1192/bjp.bp.113.131227. [ Links ]
Asociación Americana de Psiquiatría (APA) (1994). Manual diagnostico y estadístico de los trastornos mentales, Cuarta Edición (DSM-IV). Washington, DC: APA. [ Links ]
Asociación Americana de Psiquiatría (APA) (2000). Manual diagnostico y estadístico de los trastornos mentales , Texto Revisado(DSM-IV-TR). Washington, DC: APA . [ Links ]
Asociación Americana de Psiquiatría (APA) (2013). Manual diagnostico y estadístico de los trastornos mentales, 5º Edición (DSM-5). Washington, DC: APA . [ Links ]
Boeckel, M. G., Wagner, A., & Grassi-Oliveira, R. (2017).The effects of intimate partner violence exposure on the mater-nal bond and PTSD symptoms of children. Journal of Interpersonal Violence, 32 (7), 1127-1142. doi:10.1177/0886260515587667. [ Links ]
Boyer, B. A., Knolls, M. L., Kafkalas, C. M., y Tollen, L. G. (2000). Prevalence of Posttraumatic Stress Disorder in Patients with Pediatric Spinal Cord Injury: Relationship to Functional Independence. Topics in Spinal Cord Injury Rehabilitation, 6 (suppl): 125-133. doi: 10.1310/4FJ8-3VCH-EE0N-HNCD. [ Links ]
Burns, B. J., Phillips, S. D., Wagner, H. R., Barth, R. P., Kolko, D. J., Campbell, Y., y Landsverk, J. (2004). Mental health need and access to mental health services by youth involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 960-970. doi: 10.1097/01.chi.0000127590.95585.65. [ Links ]
Bustos, P., Rincón, P., y Aedo, J. (2009). Validación Preliminar de la Escala Infantil de Síntomas del Trastorno de Estrés Postraumático (Child PTSD SymptomScale, CPSS) en Niños/as y Adolescentes Víctimas de Violencia Sexual. Psykhe, 18 (2), 113-126. http://dx.doi.org/10.4067/S0718-22282009000200008. [ Links ]
Cala, M.J., Trigo, M.E., y Saavedra, F.J. (2016). Women's disengagement from legal proceedings for intimate partner violence: Sociodemographic and psychological variable. The European Journal of Psychology Applied to Legal Context, 8 (1), 35-42. Doi: 10.1016/j.ejpal.2015.10.002. [ Links ]
Carrion, V. G., Weems, C. F., Ray, R., y Reiss, A. L. (2002). Toward an empirical definition of pediatric PTSD: the phenomenology of PTSD symptoms in youth. Journal of the American Academy of Child and Adolescent Psychiatry , 41, 166-173. doi: 10.1097/00004583-200202000-00010. [ Links ]
Castro, M., Alcántara-López, M., Martínez, A., Fernández, V., Sánchez-Meca, J., & López-Soler, J. (2017). Mother’s IPV, Child Maltreatment Type and the Presence of PTSD in Children and Adolescents. International Journal of Environmental Research and Public Health, 14 (9), 1077. https://doi.org/10.3390/ijerph14091077. [ Links ]
Cedric, S, y Goldbeck, L. (2016). Consequences of the Diagnostic Criteria Proposed for the ICD-11 on the Prevalence of PTSD in Children and Adolescents. Journal of Traumatic Stress, 29, 120-123. Doi: 10.1002/jts.22080. [ Links ]
Essau, C. A., Conradt, J., y Peterman, F. (2000). Frequency, comorbidity, and psychosocial impairment of anxiety disorders in German adolescents. Journal of Anxiety Disorders, 14 (3), 263-279. doi: 10.1016/S0887-6185(99)00039-0. [ Links ]
Foa, E. B., Johnson, K. M., Feeny, N. C., y Tredwell, K. R. H. (2001). The Child PTSD Symptom Scale: a preliminary examination of its psychometric properties. Journal of Clinical Child Psychology, 30, 376-384. doi: 10.1207/S15374424JCCP3003_9. [ Links ]
Foa, E.B., Asnaani, A., Zang, Y., Capaldi, S., &Yeh, R. (2018). Psychometrics of the Child PTSD Symptom Scale for DSM-5 for Trauma-Exposed Children and Adolescents, Journal of Clinical Child & Adolescent Psychology, 47 (1), 38-46, DOI: 10.1080/15374416.2017.1350962. [ Links ]
Fong, V. C., Hawes, D., & Allen, J. L. (2017). A systematic review of risk and protective factors for externalizing problems in children exposed to Intimate Partner Violence. Trauma, Violence, y Abuse, 20 (2) 149-167. Retrieved from https://doi.org/10.1177/1524838017692383. [ Links ]
Furtado, L., Carvalhães, R., y Gonçalves, S. (2009).Violência e transtorno de estressepós-traumático na infância. (Violencia y trastorno de estrés postraumático en la infancia). Ciência & Saúde Coletiva, 14 (2), 417-433.http://dx.doi.org/10.1590/S1413-81232009000200011. [ Links ]
Gibbs, J. A. (2001). Maintaining front-line workers in child protection: A case for refocusing supervision. Child Abuse Review, 10, 323-335. doi: 10.1002/car.707. [ Links ]
Havens, J. F., Gudi, O. G., Biggs, E. A., Diamond, U. N., Weis, J. R., y Cloitre, M. (2012). Identification of Trauma Exposure and PTSD in Adolescent Psychiatric Inpatients: An Exploratory Study. Journal of Traumatic Stress , 25, 171-178. doi: 10.1002/jts.21683. [ Links ]
Howell, K. H., Barnes, S. E., Miller, L. E., & Graham-Bermann, S. A. (2016). Developmental variations in the impact of Intimate Partner Violence exposure during childhood. Journal of Injury and Violence Research, 8 (1), 43.doi: 10.5249/ jivr.v8i1.663. [ Links ]
Kolko, D. J., Hurlburt, M. S., Zhang, J., Barth, R. P., Leslie, L. K., y Burns, B. (2009). Posttraumatic stress symptoms in children and adolescents referred for child welfare investigation: A national sample of in-home and out-of-home care. Child Maltreatment, Online First. June 2009. doi: 10.1177/1077559509337892. [ Links ]
Legault, L., Anawati, M., y Flynn, R. (2006). Factors favoring psychological resilience among fostered young people. Children and Youth Services Review, 28, 1024-1038. doi: 10.1016/j.childyouth.2005.10.006. [ Links ]
López-García, J. J. y López-Soler, C. (2014).Trastorno de estrés postraumático en escolares tras el terremoto de Lorca (España) en 2011. Gaceta Sanitaria, 28 (3), 230-233.doi: 10.1016/j.gaceta.2013.10.009. [ Links ]
Manning, L., Davies, P, y Cicchetti, D. (2014). Interparental Violence and Childhood Adjustment: How and Why Maternal Sensitivity Is a Protective Factor. Childdevelopment, 85 (6), 2263-2278. doi:10.1111/cdev.12279. [ Links ]
OMS (2016). Child maltreatment (Fact sheet 150).Retrieved from http://www.who.int/mediacenter/factsheets/fs150/en/index.html. [ Links ]
Osofsky, J. D. (2003). Prevalence of Children’s Exposure to Domestic Violence and Child Maltreatment: For Implications Prevention and Intervention. Clinical Child and Family Psychology Review, 6 (3), 161-170. doi: 10.1023/A:1024958332093. [ Links ]
Oswald, S. H., Fegert, J. M., y Goldbeck, L. (2010). Post-Traumatic Stress Symptoms in Foster Children Following Maltreatment and Neglect.Verhaltenstherapie, 20, 37-44. doi: 10.1159/000274622. [ Links ]
Øverlien, C. (2010). Children Exposed to Domestic Violence. Conclusions from the Literature and Challenges Ahead.Journal of Social Work, 10 (1), 80-97. doi: 10.1177/1468017309350663. [ Links ]
Rincón, P. P., Cova, F., Bustos, P., Aedo, J., y Valdivia, M. (2010).Estrés Postraumático en Niños y Adolescentes Abusados Sexualmente. Revista Chilena de Pediatría, 81 (3), 234-240. http://dx.doi.org/10.4067/S0370-41062010000300006. [ Links ]
Scheeringa, M. S., Wright, M. J., Hunt, J. P., y Zeanah, C. H. (2006). Factors affecting the diagnosis and prediction of PTSD symptomatology in children and adolescents. American Journal of Psychiatry , 163, 644-651. doi:10.1176/appi.ajp.163.4.644. [ Links ]
Serrano-Ibáñez, E.R., Ruiz-Párraga, G.T., Esteve, R., Ramírez-Maestre, C., & López-Martínez, A.E. (2018). Validation of the child PTSD symptom scale (CPSS) in Spanish adolescents.Psicothema, 30 (1), 130-135. [ Links ]
Shenk, C. E., Putnam, F. W., y Noll, J. G. (2012). Experiential avoidance and the relationship between child maltreatment and PTSD symptoms: Preliminary evidence. Child Abuse & Neglect, 36, 118 - 126. doi:10.1016/j.chiabu.2011.09.012. [ Links ]
Tolin, D. F., y Foa, E. B. (2006). Sex differences in trauma and posttraumatic stress to disorder; to quantitative review of 25 years of research.Psychological Bulletin,132 (6), 959-992. doi: 10.1037/0033-2909.132.6.959. [ Links ]
Venta, A.C., & Mercado, A. (2019). Trauma Screening in Recently Immigrated Youth: Data from Two Spanish-Speaking Samples. Journal of Child and Family Studies, 28 (1), 84-90. https://doi.org/10.1007/s10826-018-1252-8. [ Links ]
Note: This research was carried out thanks to the following projects: “Psychological Service for Children of Female Victims of Gender Violence,” based on an agreement between the Spanish Association for the Development of Mental Health in Childhood and Youth, “I Want to Grow” and the General Management of Woman and Equal Opportunities, and the “Assessment, Diagnosis and Psychological Intervention Project for Children in Care,” based on an agreement between the University of Murcia and the General Management of Family and Social Politics
Note : Authors' participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. M.C.S. has contributed in a,b,d,e, A.M.P in d,e, C.L.-S. in a,d., J.J.L.-G. in c,d, M. A.-L. in a,b,d.
Received: July 31, 2019; Accepted: September 23, 2019











 texto en
texto en